Comment on Fraser et al, page 2867
The impact of chronic graft-versus-host disease on different aspects of overall health status and the need for prolonged therapy for this disabling complication are magnified in a joint study by the Minneapolis and City of Hope groups.
Increasing numbers of hematopoietic cell transplantations (HCTs) and improved outcomes are resulting in a growing number of survivors. Chronic graft-versus-host disease (cGVHD) is the most frequent late complication occurring after allogeneic hematopoietic cell transplantation, with reported incidence between 40% and 70%. The incidence of cGVHD is likely to increase in the future because of the increasing use of HCT in older patients, transplants from unrelated donors, peripheral blood stem cell transplants, and donor lymphocyte infusions, all of which carry a higher risk for the development of cGVHD.1 Response to current immunosuppressive therapy is unsatisfactory and leads to sustained complete response in only 50% to 60% of patients; by 2 years after transplantation, a third of the patients still have active disease, and in less than 20% of patients could immunosuppressive therapy have been discontinued.2 cGVHD and/or its treatment have been identified as the leading cause(s) of nonrelapse mortality in HCT survivors.3 Previous studies have reported (1) infection as the primary cause of mortality associated with cGVHD; (2) an association between cGVHD and reduction in performance scores, poorer quality of life, and later return to work in HCT survivors with cGVHD; and (3) the rate of physical and psychologic recovery after HCT (Syrjala et al4 and reviewed in Socie et al1 ). However, no study has assessed the impact of cGVHD on descriptive aspects of overall health.
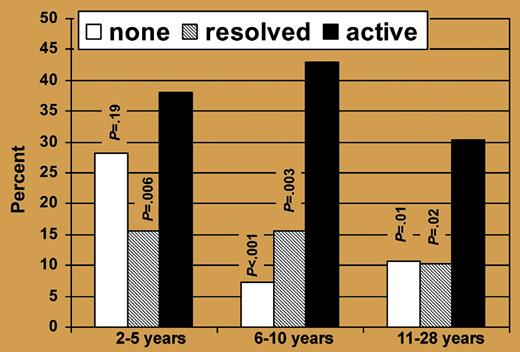
Percentage of subjects with poor or fair general health according to time since HCT and cGVHD status. See the complete figure in the article beginning on page 2867.
Percentage of subjects with poor or fair general health according to time since HCT and cGVHD status. See the complete figure in the article beginning on page 2867.
In this issue, Fraser and colleagues undertook a comprehensive analysis of the impact of cGVHD in nearly 600 individuals who had undergone allogeneic HCT, had survived 2 or more years, and had completed a 255-item health questionnaire. Global assessment of health status was measured on 6 health status domains: general health, mental health, functional impairment, activity limitation, pain, and anxiety/fear. The incidence of cGVHD in participants was 54%, of whom 46% reported active cGVHD. In multivariable analyses, subjects with active cGVHD were more likely to report adverse general health and mental health, functional impairments, activity limitation, and pain compared with those with no history of cGVHD. However, health status did not differ between those with resolved cGVHD and those who never had cGVHD.
The authors have to be congratulated for such a huge effort, and readers of Blood will be provided with a lot of quantified information (particular attention should be paid to the impressive amount of data contained in the tables). This study further highlights the need for prolonged therapy in cGVHD; 80% and 40% of the patients with active disease still needed immune suppressants 6 to 10 years and more than 10 years after transplantation, respectively.
However, while data on patient and treatment characteristics were prospectively collected, and presence or absence of cGVHD was abstracted from databases, the presence or absence of active cGVHD in the preceding year was self-reported. Subjects also self-reported whether they had taken immunosuppressant therapy for at least one month during the 2 years prior to questionnaire completion. The fact that a large proportion of the data was collected by self-report increases the likelihood of misclassification. This is further complicated by the fact that no validated quantitative criteria for organ-specific or overall responses exist, and reversible disease activity and irreversible damage may be difficult to distinguish.
Finally, data regarding extent of the disease and pattern of organ involvement were not available. This point is of obvious importance because lung or gynecologic sites, for example, have a well-known impact on general health and quality of life. It is thus difficult to draw any definitive conclusion on the second message drawn by this study—that is, “health status did not differ between those with resolved cGVHD and those who never had cGVHD” (my emphasis)—since those who had resolved disease might have had less severe disease (and/or a different pattern of involvement) than those with active cGVHD.
The use of better defined criteria for the severity and pattern of involvement recently described by the National Institutes of Health will certainly help in the future to further refine Fraser and colleagues' elegant work.
Dr Socie works with the Hôpital Saint-Louis and INSERM U728. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal