We successfully treated a 66-year-old patient with life-threatening scleromyxedema and an immunoglobulin G (IgG) lambda monoclonal spike with the BEAM regimen (BCNU, etoposide, cytarabine [Ara-C], and melphalan) and autologous stem cell transplantation (ASCT). Six months later, he had fully recovered, and at 3 years he is still asymptomatic without any other treatment, while the IgG lambda monoclonal spike is still detectable.
ASCT following treatment with high-dose melphalan alone appeared effective in 3 previous reports,1-3 although in several cases, skin lesions relapsed and had to be retreated with melphalan.
To understand the mechanisms involved in the impressive steady remission of our patient, we performed an in vitro study using the patient's fibroblasts before and after treatment. The assays demonstrated abnormal proliferation of fibroblasts before ASCT (8879 ± 398 [SD] counts per minute [cpm]) independently of soluble factors or immunoglobulins. Importantly, proliferation normalized to rates similar to that of controls (2853 ± 398 cpm) in the fibroblasts from a skin biopsy after ASCT (856 ± 90 cpm). We also incubated pre-ASCT fibroblasts with the different conditioning drugs. The proliferation reversed, after a 4-week washout, from 18 844 cpm in the untreated cultures to 1118 cpm in cultures treated with BCNU, 584.8 cpm in cultures treated with Ara-C, and 1059 cpm in cultures treated with melphalan. Previous studies using fibroblast primary cultures suggested that a serum factor stimulates fibroblasts proliferation.4 It has been reported that elimination of the monoclonal band was the cause of the improvement,1 although the isolated IgG fraction showed no stimulatory activity in a different study.5 Our patient recovered completely, although the gammopathy remains present.
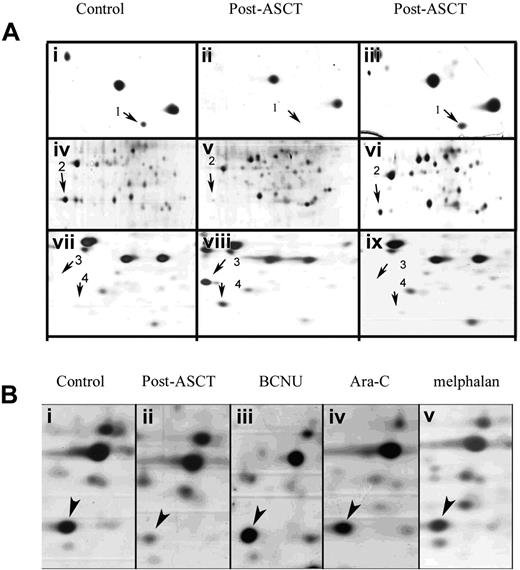
We performed a 2-dimensional (2D) analysis (BioRad, Palo Alto, CA) using fibroblast extracts from all of the previously described conditions. The Ludesi-2D Interpreter software (Ludesi, Lund, Sweden) was used for image analysis, and selected spots were analyzed using a matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF, Brukker Ultraflex, Bremen, Germany) mass spectrometer. We found several proteins that were differentially expressed between pre-ASCT and control fibroblasts. Proteins involved in growth suppression (Figure 1Aii,v,viii) were down-regulated (MnSOD,6 28-fold decrease; Cu/Zn SOD1,7 absent) in pre-ASCT fibroblasts, whereas those implicated in increased proliferation were up-regulated (stathmin,8 absent; profilin I,9 absent; and macrophage inhibitory factor,10 reduced 8.65-fold). After ASCT (Figure 1Aiii,vi,ix), all proteins that were abnormally down-regulated or up-regulated reached normal levels (ie, those observed in control fibroblasts) (Figure 1Ai,iv,vii). Interestingly, we also observed a reversal of the pre-ASCT fibroblasts'2D protein expression profile with all the drugs tested (Figure 1B).
As our patient is clinically asymptomatic and relapse-free 3 years after treatment, we propose that the pre-ASCT conditioning regimen (BEAM), which includes a combination of hypo/hypermethylating drugs, may help to avoid the relapses observed in patients treated with melphalan alone. Our results show that (1) the conditioning regimen and ASCT used in our patient can produce a permanent remission in severe scleromyxedema; (2) fibroblasts proliferate aberrantly in vitro in patients with scleromyxedema, and this can be reversed with chemotherapeutic drugs such as BCNU, Ara-C, and melphalan; and (3) monoclonal gammopathy, at least in our patient, is not responsible for the fibroblast proliferation. In conclusion, a constitutive proliferation of fibroblasts, independent of serum factors, seems to be the key pathologic feature in scleromyxedema and can be steadily reversed with the BEAM regimen in severe cases.
Differential expression of proteins associated with cell proliferation using 2D analysis. (Ai,iv,vii) Control fibroblasts; (ii,v,viii) pretreatment fibroblasts; (iii,vi,ix) posttreatment fibroblasts. These detailed pictures of the silver-stained gels demonstrate that protein expression pattern in the patient's fibroblasts after treatment mirrors that observed in control fibroblasts. Arrows identify the following proteins: (1) Cu/Zn SOD; (2) Mn SOD; (3) Profilin I; and (4) MIF. (B) Effect of the different drugs used in the conditioning procedure on the expression of MnSOD (arrowheads) in the patient fibroblasts. All drugs increased the expression of MnSOD in the patient to levels similar to control fibroblasts. (i) Control fibroblasts; (ii) patient fibroblasts untreated; (iii-v) patient fibroblasts treated with BCNU (iii), Ara-C (iv), or melphalan (v). All images were acquired with a GS-800 scanner (BioRad, Palo Alto, CA) and processed with Adobe Photoshop 7.0 (Barcelona, Spain).
Differential expression of proteins associated with cell proliferation using 2D analysis. (Ai,iv,vii) Control fibroblasts; (ii,v,viii) pretreatment fibroblasts; (iii,vi,ix) posttreatment fibroblasts. These detailed pictures of the silver-stained gels demonstrate that protein expression pattern in the patient's fibroblasts after treatment mirrors that observed in control fibroblasts. Arrows identify the following proteins: (1) Cu/Zn SOD; (2) Mn SOD; (3) Profilin I; and (4) MIF. (B) Effect of the different drugs used in the conditioning procedure on the expression of MnSOD (arrowheads) in the patient fibroblasts. All drugs increased the expression of MnSOD in the patient to levels similar to control fibroblasts. (i) Control fibroblasts; (ii) patient fibroblasts untreated; (iii-v) patient fibroblasts treated with BCNU (iii), Ara-C (iv), or melphalan (v). All images were acquired with a GS-800 scanner (BioRad, Palo Alto, CA) and processed with Adobe Photoshop 7.0 (Barcelona, Spain).

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal