Abstract
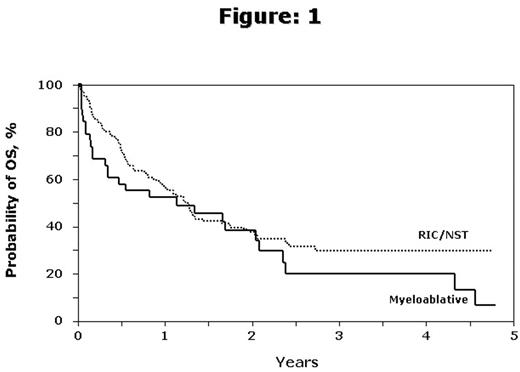
Myeloablative allogeneic HCT salvages some patients (pts) with relapsed and refractory HL but has a high treatment-related mortality (TRM). NST/RIC conditioning regimens attempt to lower TRM, in particular after previous autotransplants. We studied the outcomes of 146 patients after unrelated donor (URD) HCT with NST/RIC conditioning for relapsed and refractory HL between 1999 and 2004 reported to the CIBMTR. NST/RIC was defined following established CIBMTR criteria as TBI < 500 cGy, busulfan < 9 mg/kg, melphalan ≤ 150 mg/m2 (RIC) or fludarabine without busulfan/melphalan, TBI = 200 cGy (NST). Median (range) age was 30 yrs (13–53), 69% had a Karnofsky score (KPS) ≥ 90%, 95% patients had ≥ 3 chemo regimens prior to HCT and 89% had undergone prior autotransplant. At transplant 57 (40%) had chemosensitive disease and 74 (51%) were chemoresistant. Conditioning was RIC in 95 (65%) and NST in 51 pts (35%). At a median follow-up of 25 mo (3–64) the probability of day 100 mortality was 18% (95% CI, 12–24%), acute GVHD grade 2–4 was 61% (95% CI, 51–70%), cGVHD at 2 years was 69% (95% CI, 60–77%) and TRM at 2 years was 33% (95% CI, 25–41%). Probability of progression free survival (PFS) was 31% at 1 year and 20% at 2 years. Probability of overall survival (OS) was 56% at 1 year and 38% at 2 years (fig 1). Relapse/progression was rare after 2 years with a plateau in the survival curve. Presence of extranodal disease (relative risk [RR] 2.43, 95% CI, 1.30–4.54, p=0.006) and KPS <90 (RR 3.13, 95% CI, 1.63–6.02, p<0.001) predicted TRM. Extranodal disease (RR 2.18, 95% CI, 1.38–3.42, p<0.001), elevated serum LDH at transplant (RR 1.92, 95% CI, 1.22–3.02, p=0.001) and KPS <90 (RR 2.37, 95% CI, 1.47–3.82, p<0.001) were associated with increased risk of death. The major cause of death (45%) was progressive HL. A comparison group of 38 patients after myeloablative URD HCT between 1996 and 2004 was also analyzed. The myeloablative HCT group did not differ in age, KPS or extranodal disease, but differed in GVHD prophylaxis, previous autologous HCT (74% vs. 89% in NST/RIC, p=0.02) and stem cell source (PBSC 45% vs. 73%, p<0.001). More myeloablative HCT pts (63%) were transplanted before 2003 and a yearly increase in proportion of NST/RIC transplants was seen. Use of donor lymphocyte infusions was similar (13% of myeloablative vs 14% in NST/RIC). There was a lower risk of TRM with NST (RR 0.52, 95% CI, 0.26–1.05) and RIC (RR 0.58, 95% CI, 0.31–1.07) compared to myeloablative HCT that did not reach statistical significance. However, the given sample size had only 49% (RIC) and 39% (NST) power to detect a 20% decrease in the 2 year TRM incidence compared to myeloablative transplants. Intensity of conditioning (myeloablative vs NST vs RIC) did not affect TRM, relapse/progression, PFS and OS or death. Chemosensitivity at transplant did not predict for relapse/progression. URD HCT using NST/RIC is associated with acceptable early TRM and can salvage some heavily pretreated pts with relapsed and refractory HL.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal