Abstract
Introduction. Hodgkin’s lymphoma has a high rate of cure with current therapies; however, some patients do not respond or relapse after therapy. The aim of this study is to assess the predictive value of serum soluble Interleukin 10 (sIL-10) at diagnosis in these patients.
Patients and Methods. Two cohorts of 80 consecutive patients with Hodgkin’s lymphoma (40 male and 40 female) diagnosed and treated in the same institution were evaluated. All of them were clinically staged according to Ann Arbor system. The following parameters were evaluate for prognosis: age, sex, histology, clinical symptoms, extra-nodal disease, stage, treatment, blood counts (hemoglobin, white blood cells, lymphocyte and platelets), blood chemistry (b-2-microglobulin, tymidine-kinase and LDH levels), serum soluble IL-10 and IL-6 levels by using an ELISA method.
Statistics: Continuous variables were compared by using Wilcoxon signed-rank test, contingence tables were used for dichotomized variables; the optimal cut-off values were calculated by using CART method. Survival curves were estimated by Kaplan-Meier method and mantel-Cox were used to compare them. Cox multiple regression analysis was performed to determinate the independent contribution of the variables.Patients received COPP (n=16), hybrid schedule (n=21), ABVD (n=35), radiotherapy alone (n=6), surgery alone (n=1), and Stanford V (n=1) as first-line therapy.
Results. Median patient age was 36 years (range: 15–85 years), predominant histology was nodular-sclerosis (70%), 27 patients (34%) presented B symptoms. Bulky disease was present in 14 (17%) and bone marrow involvement in 6%. Thirty-six patients were considered as having advanced stage (II-B or II + bulky disease. III-B or III + bulky disease, and IV). The overall response rate was 92% (85% CR/CRu, and 7% PR). Eleven out of 68 patients who achieved a CR/CRu relapsed. Serum IL-10 levels were significant higher in patients with B symptoms and extra-nodal disease and correlated with β-2-microglobulin, tymidine-kinase, and (inversely) hemoglobin levels. The optimal sIL-10 serum level cut-off was established in 13.8 pg/mL. %: 54 out of 57 patients (95%), and 14 out of 23 of patients below and above this level respectively achieved a CR/CRu (P<0.001).
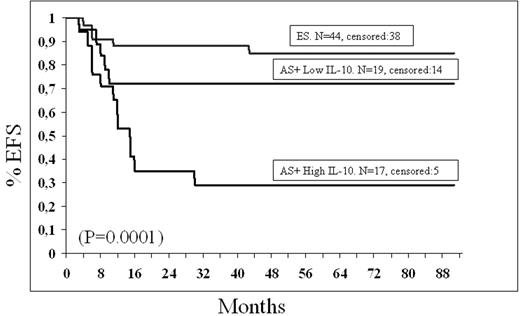
With a median follow-up of 86 months the OS and EFS are 77% and 69% respectively. Only sIL-10 > 13.8 pg/mL had independent predictive value for EFS in the multivariate analysis.
Based on this study and combining stage a serum levels of sIL-10, three subgroups could have been identify:
Patients with early disease: 85% EFS at 5 years;
patients with advanced stage (according to the above mentioned definition ) and serum levels of sIL-10 less than 13.8 pg/mL: 72% EFS at 5 years.; and
patients with advanced stage and serum levels of sIL-10 superior to 13.8 pg/mL: 29% EFS at 5 years (P=0.0001).
Conclusion. Serum levels of sIL-10 can help us to identify a subgroup of patients with advanced disease and poorer response and EFS who may benefit from more aggressive first-line therapy.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal