Abstract
Background: AML in older adults poses therapeutic challenges, as many patients are not candidates for intensive chemotherapy (IC), and it is not clear that IC provides a survival benefit compared to NIC/BSC. While risk factors and outcomes of patients treated with IC are well-defined, few data support similar prognostication in patients treated with NIC or BSC.
Methods: We conducted a retrospective review of all patients with AML receiving NIC or BSC at the Cleveland Clinic between January 1997 and December 2005. NIC consisted of treatment with hydroxyurea, low-dose cytarabine, or azacitidine. The choice and decision of therapy was dictated by patient and physician preferences. Data on known prognostic factors (age, white blood cell count (WBC) at diagnosis, cytogenetic risk groups (as defined by CALGB 8461) and AML etiology (de novo vs. secondary AML)) were collected and controlled for in multivariable analyses, and survival determined using the log-rank test, measured from the time of diagnosis. Race and residential zipcodes were obtained from information disclosed by patients in their electronic medical records. Average annual household income in a zipcode was obtained using a web-based database, www.melissadata.com.
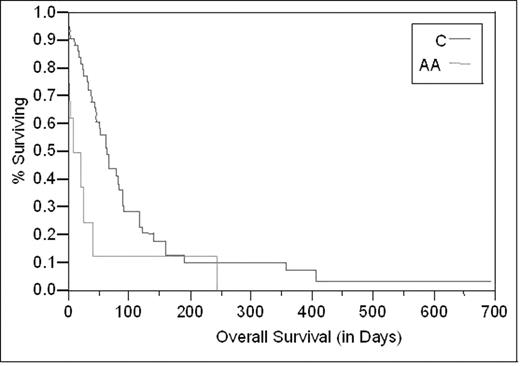
Results: Fifty-three patients were identified. The median age was 74 years (range 33–92), and 26 patients (49%) were female. Eight patients (15%) were African American (AA), while 44 patients were Caucasian (C) and 1 patient was neither AA nor C. The median WBC at presentation was 6.0 ×103/μL. Cytogenetics were favorable in 1 patient (2%), intermediate in 10 (19%), unfavorable in 19 (36%), and unknown in 23 (43%). Most patients (60%) had secondary AML. The median average annual income was $39,332 (range 23,375–82,806). The median survival was 54 days (95% CI 33–80 days) for all patients, and the 1 year survival was 7%. Known prognostic factors for AML (WBC at presentation, de novo vs. secondary AML, cytogenetics, and age at diagnosis) were not predictors of overall survival in multivariable analyses in patients not receiving intensive chemotherapy, though higher WBC count was predictive in univariable analyses. Race was a predictor for outcomes, with AA patients experiencing a worse median survival than their C counterparts (22 days versus 64 days, log rank p=0.03, figure 1) despite similar baseline characteristics. SES, however, had no impact on outcome.
Conclusions: AML patients receiving NIC or BSC have a median survival of almost 8 weeks, with AA patients experiencing worse outcomes. A small but significant percentage of patients remain alive at one year. Prognostic variables useful in treatment decision-making in patients receiving IC are less valuable for NIC/BSC patients. This information can be used for patient counseling and to help guide treatment decisions.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal