Abstract
Introduction: The diagnosis of AML and the determination of remission status depend on the percent of leukemic blasts in the bone marrow. The PPBLB is not routinely used in the diagnosis or prognosis of AML. Recently, in an analysis of patients with AML with a greater PPBLB compared to bone marrow (1/4 of the patients with AML that were studied), it was noted that a high PPBLB had a negative influence on overall survival (OS) in a univariate analysis (Amin HM. Leukemia 2005 19:1567), but this did not carry through in the multivariate analysis. We sought to examine the clinical impact of an elevated PPBLB on outcome, either early or late, in our local population of patients with AML.
Methods: All patients, previously untreated with a new diagnosis of AML admitted to the Ottawa Hospital between 2000 and 2004 were examined in this study. Patients were excluded if they had a bone marrow transplant, acute promyelocytic leukemia or secondary AML.
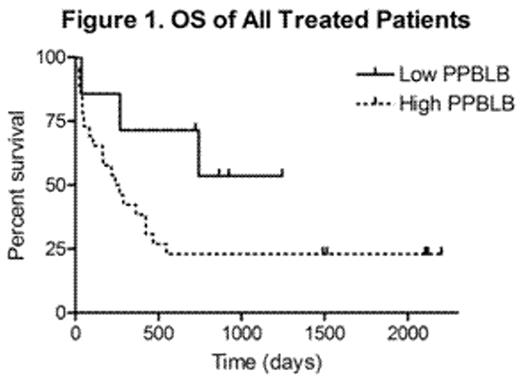
Results: 70 patients with a median age of 67.8 years were reviewed. After removing all the excluded patients only 33 received treatment (13 received 1–2 cycles of induction alone and 20 received consolidation). The median age at diagnosis was 62 years. Complete remission (CR) was achieved in 22/33 (67%) of the patients. 2 of these patients did not proceed to consolidation. The median follow-up from diagnosis in those who achieved a CR was 635 days. 6 patients died from treatment-related complications, all during induction. Upon examining OS based on the PPBLB at diagnosis it appeared that the largest differences were achieved at a cut-off of 10% PPBLB. Therefore, this cut-off was used to define high (>10%) vs. low PPBLB (<10%). Amongst the 33 patients who received treatment, 26 patients had a high PBBLB and 7 had a low PPBLB. The OS based on the PPBLB is shown in Figure 1. A trend was noted towards a lower OS with high PPBLB (p=0.1). In patients who achieved a CR (n = 22/33), 17 had a high PPBLB and 5 had a low PPBLB at diagnosis. The PPBLB was not found to be statistically significant with respect to achieving CR or early mortality but the trend favoring a low PPBLB in OS was preserved in patients who had achieved a CR (p=0.08). The PPBLB was not found to be associated with functional abnormalities of the bone marrow as determined by a lack of association with neutropenia and anemia, nor was it correlated with cytogenetics.
Conclusion: PPBLB may be predictive of long-term OS. Early mortality or the ability to achieve CR did not seem to be influenced by the PPBLB. Therefore, a high PPBLB may reflect a surrogate marker of an aggressive phenotype. This might also further support the idea that the process by which these leukemic blasts exit the bone marrow is not random or due to a “pushing” phenomenon, but rather managed by the presence or lack of adhesion molecules, coordinating this movement. Therefore, the PPBLB may be useful alone or as part of a predictive model of long-term OS of AML at diagnosis. We hope to confirm these findings in a larger patient population, exploring the impact of PPBLB on clinical outcomes.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal