Abstract
Background: Although acute GVHD (aGVHD) is a significant cause of non-relapse mortality (NRM) after allogeneic hematopoietic stem cell transplantation (HSCT), its impact on outcomes has not been fully evaluated in older patients who receive reduced-intensity HSCT (RIST).
Patients and Methods: We retrospectively surveyed the data of 334 patients (median age, 46 years: range, 1–68) with hematological malignancies who underwent allogeneic HSCT between January, 2000, and June, 2005. The diagnoses included AML/MDS (n=164), CML (n=31), ALL (n=39), lymphoma (n=95), and other malignancies (n=5). Sixty-nine patients (21%) had low- and 265 (79%) had high-risk disease. Patients were conditioned with a fludarabine-based reduced-intensity (n=169) or conventional myeloablative regimen (n=165). Patients received bone marrow (n=131), G-CSF-mobilized PBSC (n=173) or cord blood (n=30) from either an HLA-matched relative (n=138), a mismatched relative (n=41) or an unrelated volunteer (n=155). The median follow-up of surviving patients was 1,210 days (range, 346–2,317).
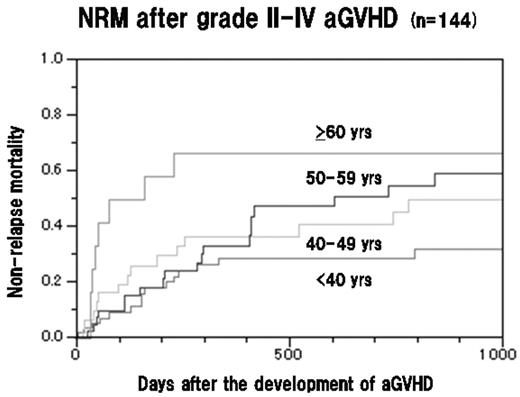
Results: Grade II-IV aGVHD occurred in 146 patients (44%; grade II, n=82; grade III, n=43; grade IV, n=21), 73 patients each in the myeloablative and RIST groups, and the timing was before disease progression or relapse in 144 patients. The incidence of NRM in these 144 patients with aGVHD was 41% (59/144), while this was 29% in the overall 334 patients. The causes of NRM included GVHD (n=22), infections with (n=19) or without (n=9) GVHD, and others (n=9). Hence, aGVHD was the primary cause of NRM. Among these 144 patients with grade II-IV aGVHD, 121 (84%) received ≥1 mg/kg/day of methylprednisone as a primary treatment for GVHD, and 19 of the 121 patients (16%) required additional treatment including switching to tacrolimus (n=11), MMF (n=9), or ATG (n=4). Subsequently, 93 patients (65%) developed chronic extensive GVHD (46 progressive and 47 quiescent). The 2-year probability of NRM after the development of aGVHD was higher as the patient age increased; i.e. 29% for <40 years, 41% for 40–49 years, 55% for 50–59 years, and 67% for ≥60 years (Figure). The 2-year NRM in patients who developed stage 2–4 gut and liver GVHD was significantly higher than that in those who did not (59% vs 30%, and 73% vs 29%, respectively). In a multivariate analysis, the maximum grade of aGVHD (HR 3.4 [95% CI, 2.3–5.1], p<0.0001), transplant from a donor other than an HLA-matched relative (HR 1.9 [95% CI, 1.1–3.4], p=0.03) and older patient age (HR 1.9 [95% CI, 1.4–2.5], p<0.0001) were associated with an increased risk for NRM after the development of aGVHD. In this analysis, disease risk and the intensity of conditioning regimens, i.e. myeloablative or reduced-intensity, were not significant risk factors for NRM.
Conclusions: Our data suggest that older patient age is a significant risk factor for NRM after the development of aGVHD, regardless of the type of conditioning regimen. The development of a careful management of aGVHD, focusing on older patients should be the subject of intense clinical research.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal