Abstract
Objective: To review the clinical and pathological profile of HIV-associated lymphomas in the local population in order to identify prognostic factors that may define a subgroup of patients who may have better outcome.
Methods: The clinical records of a cohort of 874 cases of HIV infection first seen in our institute from March 1994 to March 2006 were reviewed.
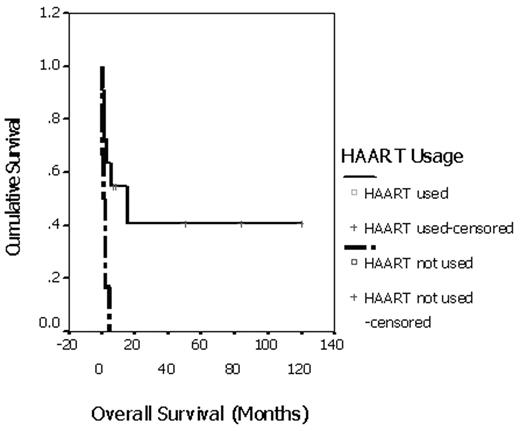
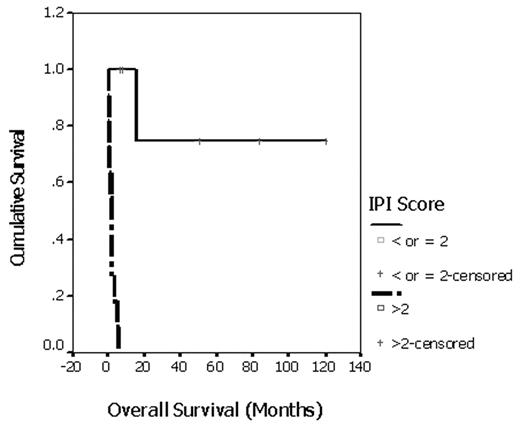
Results: Twenty patients with HIV-associated lymphomas were identified. All were males. Median age was 42 (18 – 72) years. Three had primary central nervous system lymphoma (PCNSL) and 17 had systemic non-Hodgkin’s lymphoma (NHL). All PCNSLs were of B-cell origin. For systemic NHLs, 15 patients had aggressive B-cell lymphoma (diffuse large B cell lymphoma: 12, burkitt-like lymphoma: 2, mantle cell lymphoma: 1) and 2 patients had plasmablastic lymphoma. For the 3 patients with PCNSL, 1 patient deteriorated rapidly and died 12 days after diagnosis, 1 patient survived 20 months after whole-brain radiation therapy (WBRT) and died of CMV pneumonia later and 1 patient is still surviving at 88 months (mons) after WBRT while maintaining on highly active anti-retroviral therapy (HAART). For patients with systemic NHL (n = 17), 2 patients had spontaneous disease regression upon treatment with HAART, 6 received curative intent chemotherapy, 3 received palliative treatment with chemotherapy or radiotherapy, 6 patients could not receive any treatment because of poor performance status and rapid deterioration after diagnosis. The following baseline variables were included as potential predictors of survival among all patients with systemic NHL: prior AIDS diagnosis; CD4 cell count; use of HAART and treatment intent. Number of adverse factors according to International Prognostic Index (IPI) for aggressive NHL (stage III or IV disease, age > 60 years, elevated lactate dehydrogenase, ECOG performance status ≥ 2, ≥ 2 extranodal sites) was calculated. Use of HAART was a favorable prognostic factor for overall survival (p = 0.008). Median overall survival for patients receiving HAART (n = 11) was 15 mons versus 1.6 mons for those without (n = 6). Patients with ≤ 2 adverse factors according to IPI were associated with longer overall survival (p = 0.0002). Patients with IPI > 2 (n = 11) had median survival of 2 mons whereas median survival for patients with IPI ≤ 2 (n = 6) had not been reached (range of follow up duration: 7 to 120 mons).
Conclusion: In our cohort, for patients with HIV-associated systemic NHL, use of HAART and IPI score ≤ 2 were associated with better survival.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal