Abstract
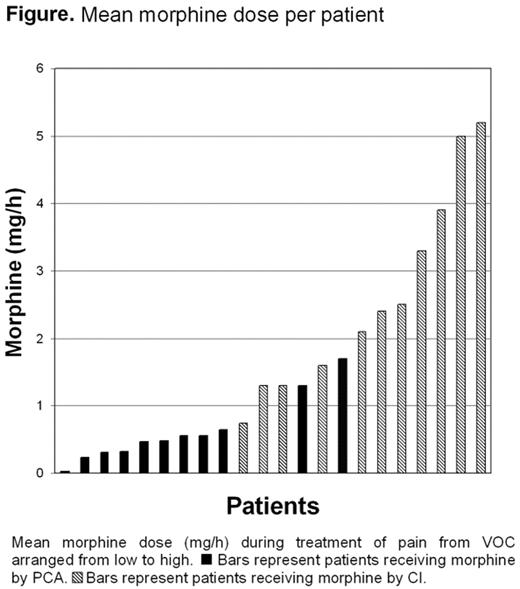
Intravenous morphine is the treatment of choice for severe pain during vaso-occlusive crisis in sickle cell disease (SCD). However, side-effects of morphine may hamper effective treatment and high plasma levels of morphine are associated with severe complications such as acute chest syndrome. Furthermore, adequate dosing remains a problem since no objective measurement of pain severity exists and analgesia should be titrated upon the patient’s reported pain. Patient-controlled analgesia (PCA) may therefore be an interesting alternative since patients can titrate the level of analgesia themselves. Although PCA is currently used for the treatment of vaso-occlusive crises in SCD, no randomized controlled trials have been performed in admitted patients with a vaso-occlusive crisis so far. In the present study, we conducted a randomized controlled trial to compare the administration of morphine with PCA versus CI in sickle cell patients with vaso-occlusive crises. Patients were randomized between PCA and CI of morphine within 24 hours after hospital admission. Endpoints of the study were: the mean and cumulative morphine dose, pain intensity, incidence of side-effects (nausea, constipation, pruritus and drowsiness) and quality of life (QoL). Pain intensity was measured daily using a ten-point-scale verbal pain score. Reduction of pain intensity was measured by subtracting a pain score on a ten point visual analogue scale (VAS) before randomization from the same measurement two days after randomization. Side-effects were measured four times per day on a 11-point numerical rating scale. QoL was measured using the 36-item Short Form Healthy Survey (SF36). Twenty five consecutive episodes of vaso-occlusive crisis in 19 patients with SCD were included in the study. No difference in the mean daily pain scores were found between the two groups (4.9 versus 5.3). However, patients in the PCA-group demonstrated to have a strongly reduced mean and cumulative morphine consumption as compared to the patients in the CI-group (0.5 mg/h versus 2.4 mg/h (P<0.001) and 33 mg versus 260 mg (P=0.018) respectively). The lower mean and cumulative morphine consumption in the PCA-group led to significant less nausea and constipation during treatment as compared to the CI-group (area under the curve respectively 11 versus 18 (P= 0.045) and 30 versus 45 (P= 0.021)). Furthermore, a non-significant reduction in the duration of hospital admission of 3 days was observed in the PCA-group. Patient controlled analgesia results in adequate pain relief at a much lower morphine consumption and should considered to be first choice in morphine administration to sickle cell patients admitted with vaso-occlusive crisis.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal