Abstract
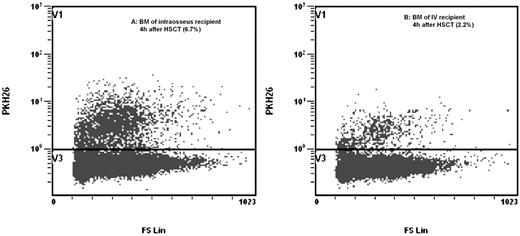
The traditional route for the delivery of hematopoietic stem cells (HSC) for transplantation by intravenous (IV) injection results in only a small percentage of the injected cells homing to the bone marrow (BM) microenvironment - where hematopoiesis could be more optimal. As such, delivery of HSCs by intra-BM injection has been investigated using syngeneic mice or autologous primate transplants. However, there has been no animal study of allogeneic HSCT directly comparing intra-BM and IV injection in terms of the seeding of donor cells in recipient BM, peripheral blood and other organs. We present the first direct comparison of donor cell homing efficiency between intra-BM and IV injection in an non-human primate (Cynomolgus Monkey) model of allogeneic hematopoietic stem cell transplant (HSCT) model using a preparative regimen modified from existing clinical protocols. Two recipients with similar age, weight and height received pre-transplant conditioning chemotherapy comprising 30mg/m2 fludarabine from Day-5 to Day-3, and 50mg/kg cyclophosphamide from Day-5 to -2. Fresh BM cells from an unrelated donor were harvested and labeled with PKH26 cell membrane dye (labeling efficiency: 99.6%) on day 0. With the recipients under general anesthesia, 2×108 donor cells were transplanted into the conditioned recipients by IV or intra-BM injection using a modified syringe suction method. Intra-BM injection recipients were found to have significantly more donor PKH26 cells, compared with IV injection recipients, in recipient BM at 2 hours (6.9% versus 2.5%, p<0.01) and 4 hours (6.7% versus 2.2% p<0.01) after transplantation. There were somewhat fewer donor cells in the peripheral blood after intra-BM delivery (3.4% versus 4.6%) at 2 hours, though the percentages were the same 4 hours after injection (1.6% in both). Interestingly, donor cell percentages in the bone marrow remained stable between 2 to 4 hours after transplant, as opposed to donor cell percentages in the peripheral blood, which fell by 2.1 to 2.9 times between 2 to 4 hours after transplant. Furthermore, compared to IV injection, intra BM injection retained more cells within BM, with less cells trapped in other organs, like the spleen (1.4% vs. 3.1%) and liver (0.8% vs. 3.5%), as well as non-hematopoietic organs like the heart (1.1% vs. 4.9%), lung (1.0% vs. 4.0%) and kidney (1.5% vs. 3.2%). Our study showed that in a allogeneic non-human primate model of HSCT, intra-BM injection of HSC resulted in superior retention of donor cells in BM with reduced seeding onto non-hematopoietic organs - suggesting possible applications for improved donor cell engraftment and reduced effects of donor-cell-mediated graft versus host disease on non-hematopoietic organs.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal