Abstract
Background: Renal insufficiency of varying severity including end stage renal disease requiring dialysis is often a presenting manifestation of multiple myeloma (MM). While many patients (pts) improve following initiation of therapy for MM, a considerable number of pts proceed to stem cell transplant with less than optimal renal function. It is not clear whether the outcome of their transplants differs from pts with normal renal function.
Methods: The MM transplant database was searched to identify pts with a Creatinine clearance (Crcl) of less than 50 ml/min/m2 (study cohort). These pts were then matched to two pts each with a clearance of ≥ 50 ml/min/m2 (control cohort), based on cytogenetic abnormalities (normal vs. abnormal), circulating plasma cells (yes vs. no), age at transplant, % of plasma cells at transplant, plasma cell labeling index, time to transplant from diagnosis and the disease status at transplant, the factors used in that order of importance.
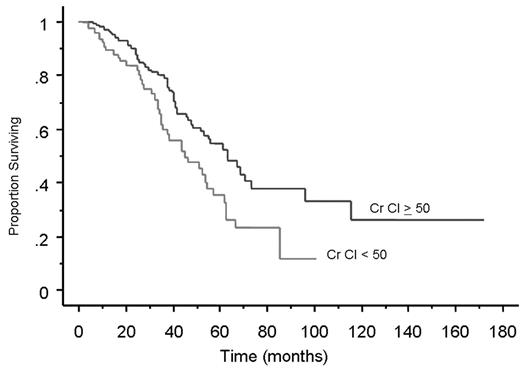
Results: Eighty pts with a Crcl < 50 ml/min were identified and matched to 160 pts with Crcl ≥ 50 ml/min. The pts were matched for the above factors and the two groups were similar in terms of their other baseline features except CRP and B2M, both of which were lower in the control group. Pts with reduced renal function were more likely to receive dose reduced melphalan for conditioning (32.5%) compared to the control group (2%; P < 0.0001). The outcomes from the stem cell transplant were similar in both the groups. 96% of pts obtained an objective response to stem cell transplant in each of the groups with no difference in the time to response; and a complete response was seen in 38.5% and 36.6% of the study and control cohorts respectively (P=NS). The median post transplant progression free survival was 18.2 months and 18.4 mos respectively for the study cohort and the control group (P=0.4). However, the median overall survival from transplant was shorter for the study cohort (30.7 mos vs. 60 mos for the controls; P = 0.007; Figure). The time to platelet and neutrophil engraftment was not different between the groups. In terms of transplant related toxicity, the median days hospitalized was higher in the study group (5 days vs. 9.5 days; P=0.003) as was the incidence of grade 3 and 4 mucositis (8% vs. 23%; P= 0.0008). Six pts (7.5%) had treatment related deaths in the study group compared to 3 pts (2%) among the controls (P=0.03), the majority of the deaths being infection related.
Conclusion: Here we demonstrate that pts with MM and reduced renal function derive disease free survival comparable to those with normal renal function, despite the increased use of reduced dose Melphalan for conditioning. The toxicity is clearly increased in the presence of abnormal renal function. Interestingly, the overall survival was inferior among the pts with reduced renal function. One possible explanation for this observation is the decreased availability of novel therapies for salvage among pts with reduced renal function as many of them would not be eligible for clinical trials due to reduced renal function.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal