Abstract
Despite increases in CR rates, most patients with AML will relapse following successful induction treatment. Allogeneic stem cell transplantation (SCT) remains the most effective post-induction relapse preventing treatment. Similarly, for patients with relapsed/chemorefractory disease, SCT represents the only possible curative treatment modality. However, because of the significant morbidity and mortality of myeloablative conditioning regimens, SCT has been mainly restricted to young patients without co-morbidities. Because of these limitations, currently most transplant centers limit the application of SCT to patients younger than 50–55 years old.
This study included 73 patients (M=37, F=46, median age 39-years, range (17–65)) with AML treated with a single nonmyeloablative (NST) regimen in the BMT department of Hadassah University Hospital. The majority of patients had advanced AML pre-transplant (CR1 n=27; CR2 n=14; CR3 n=1; relapse n=31; chemorefractory disease n=24). All patients were prepared by the NST protocol that included IV fludarabine 30mg/m2/day (on days -10 to -5) and oral busulfan 4mg/kg/d or IV busulfex at a dose of 3.2 mg\kg\d (on days -6 and -5), with IV ATG (on days -4 and -1).
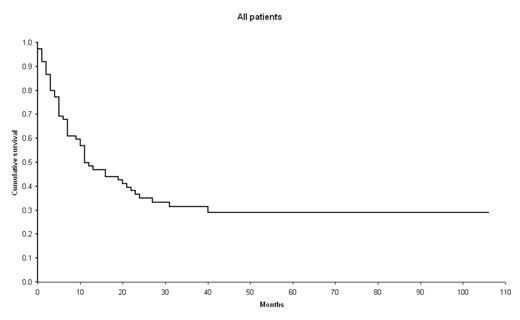
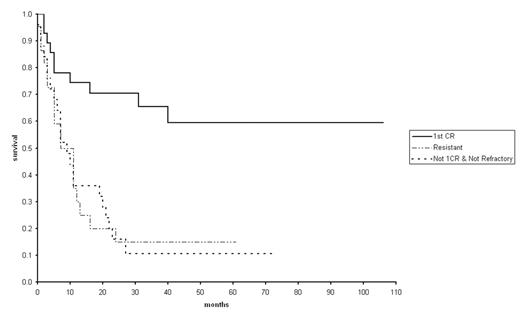
Results: Engraftment of neutrophils was achieved in 70/73 (96%) patients within a median of 15 (range 9–31) days, while engraftment of platelets was achieved in 69/73 patients (95%) within a median of 12 (range 0–86) days. Chimerism analysis data were available for 68 patients. Complete donor chimerism in the peripheral blood was achieved in 58/68 (85%) patients. 42/68 patients (62%) who survived at least one month and had a sustained engraftment, developed aGVHD. The cumulative incidence of severe aGVHD grade III-IV was 27% (18/68 patients). 35/65 (54%) patients who survived more than 100 days developed cGVHD, which was extensive in 22 (34%) cases. The cumulative incidence of NRM at 100d and 1y was 12% and 28% respectively. With a median follow up of 38m (range 10 – 118), 24/73 patients survived. Twenty-one patients survive in continuous CR, while 3 patients who relapsed post-transplant survive in CR after a second allo-SCT. The estimated long-term OS for the whole group is 30% (figure 1). 27/73 patients underwent transplantation while in CR1. Two out of these 27 patients relapsed and died, while another 8 patients died due to transplant associated complications. The estimated long-term OS for this subgroup is 63% (17/27 patients surviving in continuous CR) (figure 2).
In conclusion, the results of our study showed that our NST approach is associated with a potent anti-leukemic efficacy. The results of our study look comparable to those obtained after standard myeloablative conditioning even when stratified into disease status subgroups. Prospective randomized trial comparing myeloablative vs nonmyeloablative regimens low-risk patients is warranted.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal