Abstract
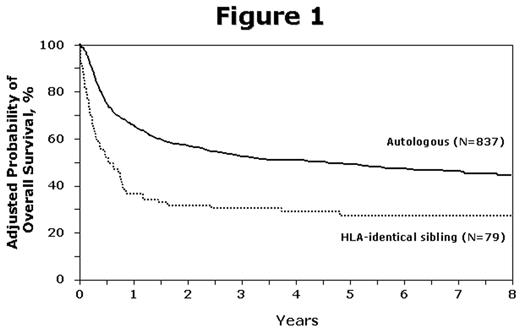
No randomized trials have compared autologous HCT (autoHCT) to allogeneic HCT (alloHCT) for DLBCL. We analyzed the outcomes of 916 patients (pts) (837 autoHCT and 79 alloHCT) ages 18–60yrs after a first autoHCT or HLA-identical sibling alloHCT for DLBCL between 1995 and 2003 reported to the CIBMTR. Pts receiving T-cell depleted allografts or reduced-intensity conditioning were excluded. There were significant baseline differences between the groups in disease stage, B symptoms, extranodal disease and marrow involvement. AlloHCT pts were significantly more likely to have >3 chemo regimens prior to HCT (53 vs 40%), and resistant induction failure or relapse (39 vs 16%). At 1yr, treatment-related mortality (TRM) was higher after alloHCT (41%, 95% CI, 30–52%) than after autoHCT (11%, 95% CI, 9–14%, p<0.001), but risks of relapse/progression were similar (30%, 95% CI, 21–41%) and (33%, 95% CI, 29–36%, p=0.69), respectively. Cumulative incidence of outcomes and univariate probabilities of progression free (PFS) and overall survival (OS) at 5 yrs are summarized in table 1. In multivariate analysis, allo and autoHCT had differential early and late effects on outcomes. In the first 12 mo after transplant, alloHCT was associated with higher TRM (RR 4.76, 95% CI, 3.14–7.22, p<0.001), treatment failure (RR 2.08, 95% CI, 1.56–2.77, p<0.001) and mortality (RR 2.78, 95% CI, 2.06–3.77, p<0.001) but similar risk of progression (RR 1.14, 95% CI, 0.75–1.74, p=0.54) compared to autoHCT. Among pts surviving 12 mo post-transplant, no significant difference was observed between autoHCT and alloHCT for TRM, progression, PFS, or OS. Covariates that increased the risks of TRM and OS were older age (51–60 years), KPS <90%, chemoresistance at transplant, and earlier transplant yr (before 2001 vs later). Older age and chemoresistance were also associated with progression and lower PFS. There were no significant interactions between graft type and other prognostic variables; in particular, relative risk of outcomes with allo vs autoHCT were similar for patients with chemosensitive and chemoresistant disease. In summary, myeloablative alloHCT increased risks of early TRM and mortaliy without an effect on progression (compared to autoHCT). Transplant type did not affect outcomes after 12 months post-transplant. AutoHCT was associated with superior survival (fig 1), and the difference was not explained by differences in chemosensitivity at the time of transplant.
| . | AutoHCT . | AlloHCT . |
|---|---|---|
| Outcomes | (95%CI) | (95%CI) |
| AGVHD @ day 100 | N/A | 42 (31–53) |
| CGVHD @ 5yrs | N/A | 27 (18–38) |
| TRM @ 5yrs | 18 (15–20) | 45 (34–57) |
| Relapse/progression @ 5yrs | 39 (36–43) | 33 (23–44) |
| PFS @ 5yrs | 43 (40–46) | 26 (18–37) |
| OS @ 5yrs | 49 (46–53) | 27 (18–27) |
| . | AutoHCT . | AlloHCT . |
|---|---|---|
| Outcomes | (95%CI) | (95%CI) |
| AGVHD @ day 100 | N/A | 42 (31–53) |
| CGVHD @ 5yrs | N/A | 27 (18–38) |
| TRM @ 5yrs | 18 (15–20) | 45 (34–57) |
| Relapse/progression @ 5yrs | 39 (36–43) | 33 (23–44) |
| PFS @ 5yrs | 43 (40–46) | 26 (18–37) |
| OS @ 5yrs | 49 (46–53) | 27 (18–27) |
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal