Abstract
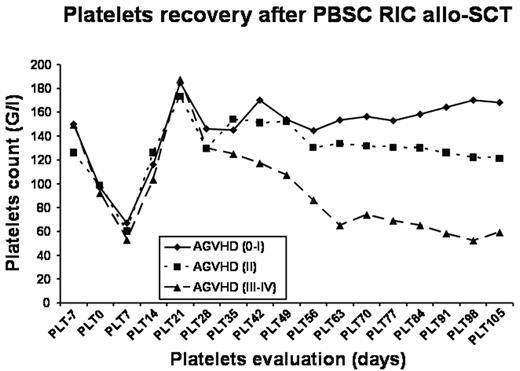
Few data are currently available regarding platelets trasfusion needs and the kinetics and predicitive factors for platelets recovery after RIC allo-SCT. In this study, we analyzed the profile of platelets recovery and transfusion needs in the first 100 days after sibling PBSC RIC in a single institution series of 166 consecutive transplantations. Patients and graft characteristics were: age 49 y. (range: 18–70), diagnoses: 66 myeloid malignancies (40%), 64 lymphoid malignancies (39%), and 36 metastatic solid tumors (21%). 112 pts (67%) received an ATG-based RIC, while 54 pts (33%) received a low dose irradiation-based RIC. 75 pts (45%) developed grade 2–4 acute GVHD. Platelets recovery (>20 G/L) was observed at a median of 9 days (range: 0–99). The kinetics profile of platelets recovery is shown in the figure below. In the whole study population, the nadir was observed around day +7 after allo-SCT, and a plateau was reached about day +35. Filtered and irradiated donor apheresis platelets were used and patients needed a median of 1 unit (range: 0–53). In this series, 83 pts (50%) did not require any platelets transfusion during the follow-up period (median follow-up: 442 days) and 83 patients (50%) received at least one transfusion of platelets (54 were not transfused beyond day +100 after allo-SCT). Platelets count prior to RIC allo-SCT (median count 144 G/L; HR 0.44 (0.28–0.7) p=0.002), conditioning regimen (use of ATG; HR 1.86 (1.08–3.2) p=0.025) and the occurrence of acute (HR 1.54 (1.17–2.01); p=0.001) and severe GVHD (HR 2.36 (1.38–3.05) p=0.0006; 82% of patients with grade 3–4 acute GVHD were transfused) were the parameters significantly associated with platelets transfusion needs in multivariate analysis. In this cohort, 145 pts could be assessed for platelets recovery at day +100: among them, 99 (68%) had a platelet count >99 G/L. Univariate analysis found a significant impact of acute GVHD (p=0.0001) and platelet count prior to conditioning (p=0.012) but only acute GVHD (HR 5.52 (2.48–12.25); p=0.001) was associated with a delayed platelet recovery in a multivariate model. No impacts of pathology, GVHD prophylaxis regimen or CD34+ cell dose were demonstrated.
Overall, these observations show a significantly lower rate of platelets transfusions and a quicker kinetic of platelets recovery after RIC allo-SCT and point out the effect of acute GVHD. In addition, considering the low level of myeloablation observed, RIC could be an appropriated field of investigation for the testing of megakaryocytic stimulating agents, towards further improving the safety and outcome of RIC allo-SCT.
Platelets recovery after PBSC RIC allo-SCT
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal