Abstract
Efficacy and safety of azacitidine (Vidaza®), at the FDA-approved dosing schedule of 75 mg/m2/day x 7 days every 28 days, was demonstrated in a phase III CALGB study by Silverman et al (
JCO 2002; 20:2429
) for the treatment of myelodysplastic syndromes (MDS). The objective of this phase II, multicenter, randomized, open-label study in all FAB subtypes of MDS was to study the treatment response and safety of 3 alternative subcutaneous azacitidine dosing schedules, eliminating the need for weekend azacitidine injections. Patients were randomized to either AZA 5-2-2 (75 mg/m2 day x 5 days, followed by 2 days no treatment, followed by 75 mg/m2/day x 2 days), AZA 5-2-5 (50 mg/m2/day x 5 days, followed by 2 days no treatment, followed by 50 mg/m2/day x 5 days) or AZA 5 (75 mg/m2/day x 5 days). After 6 cycles of azacitidine, patients meeting International Working Group MDS response/improvement criteria (Blood 2000; 96:3671
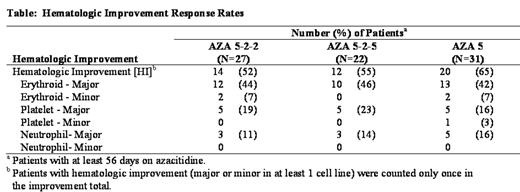
), defined as complete remission, partial remission, stable disease, or hematologic improvement, were eligible to receive an additional 12 cycles. As of July 1st, a total of 106 patients have been randomized in the AZA 5-2-2 (n=33), AZA 5-2-5 (n=35), and AZA 5 (n=38) treatment arms. Based on FAB classification, most patients have RA (42%, 45/106) or RAEB (30%, 32/106). Of 80 patients who have received ≥2 cycles of treatment, hematologic improvement (major or minor in at least 1 cell line) occurred in 58% (46/80) of the patients (Table). Median time to improvement in the 3 arms ranged between 1 and 3 cycles (AZA 5-2-2: 1.1, AZA 5-2-5: 3.0, AZA 5: 2.6). Of 38 patients who were RBC transfusion dependent at baseline, 27 (71%) became independent (AZA 5-2-2: 59%, 10/17, AZA 5-2-5: 89%, 8/9; AZA 5: 75%, 9/12). The most common grade 3 or 4 events included neutropenia 29%, 28/98 (AZA 5-2-2: 44%, 14/32; AZA 5-2-5: 20%, 6/30, and AZA 5: 22%, 8/36), thrombocytopenia 15%, 15/98 (AZA 5-2-2: 28%, 9/32; AZA 5-2-5: 10%, 3/30, and AZA 5: 8%, 3/36) and anemia 12%, 12/98 (AZA 5-2-2: 16%, 5/32; AZA 5-2-5: 17%, 5/30, and AZA 5: 6%, 2/36). The frequency of patients with a grade 3 or 4 infection was 15%, 15/98 (AZA 5-2-2: 19%, 6/32; AZA 5-2-5: 23%, 7/30; AZA 5: 6%, 2/36) or hemorrhage was 4%, 4/98 (AZA 5-2-2: 6%, 2/32; AZA 5-2-5: 7%, 2/30; AZA 5: 0/36). Updated data will be available at the time of the meeting. Based on preliminary results, these data indicate that the 3 alternative dosing schedules provide clinical benefit (i.e., transfusion independence and hematologic improvement) and are consistent with the FDA-approved 75 mg/m2/day x 7 days dosing results from previous CALGB studies.Disclosures: Yes, dosing regimens are different from the approved prescribing information.; Heidi McIntyre, CL Beach and Jay Backstrom are employees of Pharmion Corporation.; Roger Lyons.; Heidi McIntyre, CL Beach, Jay Backstrom.; Roger Lyons.; Thomas Cosgriff - discussion leader.; Roger Lyons - advisory committee.
Author notes
*
Corresponding author
2006, The American Society of Hematology
2006

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal