Abstract
Background. Recent studies suggest that Flow Cytometry (FCM) might provide information useful in managing Myelodysplastic Syndromes (MDS) patients.
Aim of the work. The purpose of this work is to describe the prognostic relevance of FCM analysis on a cohort of 303 myelodysplastic patients (64 RA; 15 RARS; 59 RCMD; 12 5q-MDS; 20 U-MDS, 72 RAEB-I, 44 RAEB-II, 17 LMMC), registered in the Multicenter Piedmont MDS Registry.
Patients, materials, and methods. Marrow of 303 patients was studied by seven local FCM laboratories, using monoclonal antibodies against: CD3, CD8, CD4, CD16, CD19, CD34, CD117, CD33, CD14, CD11b, CD66b, HLADR, GPA and CD45. Myeloid maturation was evaluated according to the expression of both CD11b and CD66b antigens. Immature compartment of myeloblasts was analysed with CD117 and CD11b−CD66b−, and myeloid maturation with CD11b−CD66b+ (promyelocytes), CD11b+CD66b++ (myelocytes and metamyelocytes), CD11b+CD66b+ (neutrophils and bands). This definition of myeloid subpopulations was confirmed by sorting and by citospin. The overall survival (OS) and Leukemia-Free Survival (LFS) was calculated from the time of diagnosis until death or until leukaemia transformation. Survival curves were obtained by the Kaplan-Meier method and compared by the log-rank test. To evaluate the impact of FCM parameters on OS and LFS, we determined quantitative expression of the following antigen: CD117 and CD11b−CD66b− (≤5% vs >5%); CD11b−CD66b+ (≤12% vs >12%); CD11b+CD66b++ (≤15% vs >15%); CD11b+CD66b+ (≤25% vs >25%).
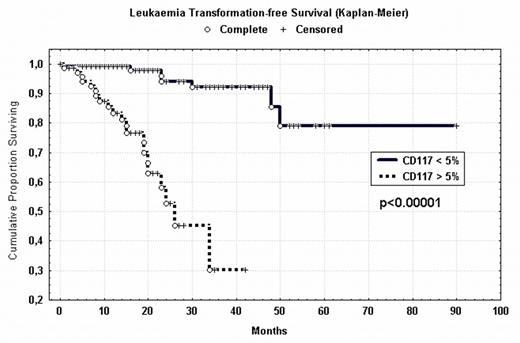
Results. In our patients, quantitative expression of CD117 correlated with a shorter OS and LFS: the 40 months-OS was 66,5% versus 26,4% (p<0.00001) while LFS was 91.6% versus 27.6% (p<0.00001) (Fig 1). Similarly OS and LFS decreased when CD11b−CD66b− (myeloblasts) increased. Conversely, we observed a higher OS and LFS in patients with a high percentage of subpopulations CD11b+CD66++ and CD11b+CD66+ (Table 1).
Discussion. Cytometric recognitions of dysplasia is difficult to perform, as it requires subjective interpretation by a skilled pathologist. This study emphasizes that FCM analysis of myeloid maturation, expressed as percentage of positive cells, may provide meaningful prognostic information. Both blast percentage expressed as CD117+ or CD11b−CD66b− and the quantitative assessment of myeloid lineage maturation showed, in our experience, a high prognostic value. These FCM parameters should be proposed as a prognostic tool easy to reproduce and perform.
Results of quantitative FCM markers
| FCM variable . | Cut off . | 40 months-OS . | p . | 40 months-LFS . | p . |
|---|---|---|---|---|---|
| CD117+ | ≤5% vs >5% | 66.5% vs 26.4% | 0.00001 | 91.6% vs 27.6% | 0.00001 |
| CD11b−CD66b− | ≤5% vs >5% | 71.5% vs 45.9% | 0.0002 | 90.8% vs 51.3% | 0.00001 |
| CD11b−CD66b+ | ≤12% vs >12% | 49.8% vs 58.1% | NS | 80.7% vs 76.6% | NS |
| CD11b+CD66++ | ≤15% vs >15% | 33.0% vs 63.3% | 0.001 | 58.9% vs 87.5% | 0.002 |
| CD11b+CD66b+ | ≤25% vs >25% | 30.3% vs 64.3% | 0.00003 | 53.3% vs 76.6% | 0.0008 |
| FCM variable . | Cut off . | 40 months-OS . | p . | 40 months-LFS . | p . |
|---|---|---|---|---|---|
| CD117+ | ≤5% vs >5% | 66.5% vs 26.4% | 0.00001 | 91.6% vs 27.6% | 0.00001 |
| CD11b−CD66b− | ≤5% vs >5% | 71.5% vs 45.9% | 0.0002 | 90.8% vs 51.3% | 0.00001 |
| CD11b−CD66b+ | ≤12% vs >12% | 49.8% vs 58.1% | NS | 80.7% vs 76.6% | NS |
| CD11b+CD66++ | ≤15% vs >15% | 33.0% vs 63.3% | 0.001 | 58.9% vs 87.5% | 0.002 |
| CD11b+CD66b+ | ≤25% vs >25% | 30.3% vs 64.3% | 0.00003 | 53.3% vs 76.6% | 0.0008 |
Leukaemia transformation free Survival (Kaplan-Meier) ○ Complete + Censored
Leukaemia transformation free Survival (Kaplan-Meier) ○ Complete + Censored
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal