Abstract
MDS/MPD-U is a newly defined clinical entity in the WHO classification. It includes patients (pts) with features of both myelodysplasia and myeloproliferation that cannot be classified under any other WHO category. In addition it includes the provisional entity RARS-T. Recent reports found an increased incidence of JAK-2 mutation in pts with RARS-T, suggesting possibly a different biological behavior. The clinical outcome of MDS/MPD-U, and in particular RARS-T, pts have not been well described.
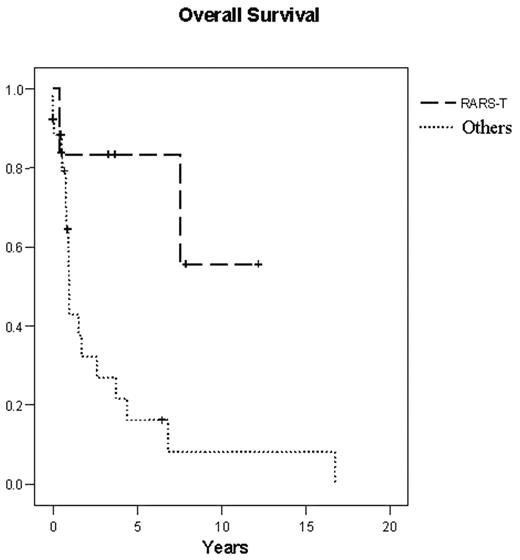
We reviewed 142 patients in the MD Anderson Leukemia Department patient database with the diagnosis of MDS/MPD or MPD-U seen from September 1987 to July 2006, and identified 32 pts that fulfilled MDS/MPD-U criteria according to WHO classification. The median age was 64 years (range 21–82), with a male: female ratio of 3:1. Six pts had RARS-T (19%). Six pts had a previous malignancy (19%), of which 3 received radiation therapy; no chemotherapy was given. Twenty-five pts (73%) were symptomatic at presentation, including fatigue in 17 (53%), weight loss in 13 (41%), fever in 2 (6%), and night sweats in 7 (22%) pts. Fifteen (45%) pts were transfusion dependent. The median hemoglobin was 9.6 g/dl (range 4.8–15.3), white blood cell count 9x109/L (range 0.6–141), platelets 234x109/L (range 7–1687), and percentage of bone marrow blasts 3% (range 0–16). Fifteen pts (45%) had more than one lineage dysplasia and 22 pts (69%) had increased reticulin in the bone marrow. Cytogenetic analysis revealed diploid cytogenetics in 13, trisomy 8 (either alone or with other abnormalities) in 8, complex cytogenetics in 3, and others in 8 pts. Twenty-two pts were treated with multiple different therapies, including hypomethylating agent in 8, with no sustained responses to any therapy. Six pts received supportive care only and 4 are unknown. Two pts underwent bone marrow transplant; one is in remission for >4 years and the other died from acute graft versus host disease. Median follow up time for alive pts was 10.6 months (range 0.3–147). Median survival of the whole group was 19 months (95% CI; range 8–29). Of the 6 pts with RARS-T, 5 had diploid cytogenetics, two had prior malignancy and 5 were transfusion dependent at the time of diagnosis. Patients with RARS-T had a significantly better survival than the other pts (median survival not reached vs. 12 months; p=0.019; Figure 1).
In conclusion, pts with MDS/MPD-U have a poor prognosis with a median survival of one year. However, RARS-T represents a subgroup of pts with better prognosis and long overall survival justifying their separate categorization.
Overall Survival
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal