Abstract
Imatinib and recombinant interferon alpha (rIFNα) can induce remission in polycythemia vera (PV) patients, but gauging the depth of responses has not been possible due to lack of a specific disease marker. We found that patients undergoing imatinib (n = 14) or rIFNα (n = 7) therapy remained strongly positive for V617F JAK2, although there was a significant reduction in the median percentage of mutant alleles that correlated with hematologic response (P = .001). Furthermore, individuals who achieved complete hematologic remission had lower levels of V617F than those who did not (P = .001). Of 9 imatinib-treated cases for whom pretreatment samples were available, 7 with no or partial hematologic responses showed a marginal increase (median, 1.2-fold; range, 1.0-1.5) in the percentage of V617F alleles on treatment, whereas the 2 patients who achieved complete hematologic remission showed a 2- to 3-fold reduction. Our data indicate that, although PV patients may benefit from imatinib or rIFNα, molecular responses are relatively modest.
Introduction
Polycythemia vera (PV) is a myeloproliferative disease characterized by an increased red-cell mass and usually an increase in megakaryocytes in the bone marrow and platelets in the peripheral blood. Untreated, the disease leads to thrombohemorrhagic complications and in most cases to progressive marrow myelofibrosis, anemia, and splenomegaly.1 Long-term remission has been reported with recombinant interferon alpha (rIFNα),2-7 and, more recently, a number of patients have achieved complete or partial responses after treatment with imatinib mesylate.8-11
rIFNα has been reported to induce cytogenetic remission in occasional patients and/or result in conversion of monoclonal to polyclonal hematopoiesis.3 Such events have not been reported as yet following imatinib treatment. However, since only 20% of patients present with a chromosomal abnormality, it has not been possible, in general, to gauge the depth of responses to treatment. Here, we have exploited the recently described V617F JAK2 mutation12-18 as a disease marker to measure the response of PV patients to rIFNα or imatinib.
Study design
Patients
We studied 111 PV patients, of whom 21 had undergone treatment in 2 larger sequential phase 2 single-institution studies. Seven patients received rIFNα in the first study (initial doses 1 MU 3 times weekly to 3 MU daily; median follow-up, 60 months; range, 13-132), and 14 received imatinib in the second study (initial doses 400 to 800 mg daily; median follow-up, 17 months; range, 5-31). The 90 remaining patients, constituting the control group, were either untreated or treated by phlebotomy only, hydroxyurea, and/or anagrelide. For rIFNα-treated cases, complete hematologic response (CR) was defined as no need for phlebotomy, a sustained hematocrit level of less than .45 (45%) for men and less than .42 (42%) for women, and platelet count of 600 × 109/L or less. Partial hematologic response (PR) was the aforementioned but platelet count ranged between 600 and 1000 × 109/L (Polycythemia Vera Study Group criteria). For imatinib-treated patients, CR was defined as phlebotomy-free within the first 18 months of treatment, hematocrit level of .45 (45%) or less for men and .42 (42%) or less for women, platelet count of 400 × 109/L or less, and absence of splenomegaly if spleen was initially palpable. PR was defined as phlebotomy-free within the first 18 months, hematocrit level of .45 (45%) or less for men and .42 (42%) or less for women, platelet count more than 400 × 109/L, and spleen reduced to 50% or less of the original size, if initially palpable. All responses were thus considered quantitative, not qualitative. The studies had been approved by the internal review boards from participating institutions and informed consent was provided according to the Declaration of Helsinki.
Molecular studies
DNA was extracted from peripheral-blood samples (n = 111) by standard procedures after isolation of total leukocytes or granulocytes following red-cell lysis or by density gradient centrifugation over Histopaque 1077 (Sigma-Aldrich, Ayrshire, United Kingdom). DNA was also extracted from pretreatment, unstained bone marrow slides (n = 9). V617F was detected initially using an amplification refractory mutation system (ARMS) assay as described.17 The proportion of mutant alleles (%V617F) was quantified using pyrosequencing as detailed,17 except that samples were amplified using primers 5′-TCTTTGAAGCAGCAAGTATGA-3′ and 5′-biotin-GCCTGTAGTTTTACTTACTCTCG-3′ and sequenced with primer 5′-TTTTAAATTATGGAGTATGT-3′. Comparison of the %V617F between control and treated patients was performed using the Mann-Whitney test.
Results and discussion
Using ARMS, V617F was detected in 82 (91%) of the control PV cases and in all 21 cases undergoing treatment with imatinib or rIFNα. The sensitivity of the assay is approximately 5%,17 indicating that neither therapy had reduced the percentage of mutant cells below this level. Patient details and results are summarized in Table 1.
Summary of patient characteristics and results for cases undergoing therapy with imatinib or rIFNα
Patient no. . | Sex . | Age at diagnosis, y . | Rx . | Dose . | F/U, mo . | Response . | % V617F on treatment . | % V617F before treatment . |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 26 | Imatinib | 800 mg/d | 5 | NR | 44 | ND |
| 2 | F | 60 | Imatinib | 700 mg/d | 5 | PR | 41 | 34 |
| 3 | M | 49 | Imatinib | 800 mg/d | 9 | NR | 89 | 71 |
| 4 | F | 67 | Imatinib | 500 mg/d | 9 | PR | 91 | 88 |
| 5 | M | 58 | Imatinib | 400 mg/d | 10 | PR | 72 | ND |
| 6 | M | 48 | Imatinib | 800 mg/d | 15 | PR | 57 | 40 |
| 7 | M | 31 | Imatinib | 800 mg/d | 17 | PR | 76 | 63 |
| 8 | F | 48 | Imatinib | 500 mg/d | 17 | CR | 8 | 25 |
| 9 | F | 28 | Imatinib | 800 mg/d | 19 | PR | 83 | 82 |
| 10 | M | 72 | Imatinib | 400 mg/d | 21 | NR | 72 | ND |
| 11 | M | 54 | Imatinib | 300 mg/d | 24 | CR | 21 | 44 |
| 12 | M | 43 | Imatinib | 400 mg/d | 25 | PR | 60 | 40 |
| 13 | M | 30 | Imatinib | 600 mg/d | 25 | PR | 19 | |
| 14 | M | 53 | Imatinib | 700 mg/d | 31 | PR | 30 | ND |
| 15 | F | 32 | rIFNα | 3 MU 3 times/wk | 13 | CR | 19 | ND |
| 16 | F | 39 | rIFNα | 3 MU 5 days/wk | 45 | CR | 39 | ND |
| 17 | M | 53 | rIFNα | 3 MU/day | 50 | CR | 29 | ND |
| 18 | F | 48 | rIFNα | 4 MU, alternate d | 60 | PR | 87 | ND |
| 19 | M | 42 | rIFNα | 2 MU 3 times/wk | 60 | CR | 27 | ND |
| 20 | M | 52 | rIFNα | 4.25 MU 3 times/wk | 108 | CR | 22 | ND |
| 21 | M | 39 | rIFNα | 3.5 MU/d | 132 | CR | 25 | ND |
Patient no. . | Sex . | Age at diagnosis, y . | Rx . | Dose . | F/U, mo . | Response . | % V617F on treatment . | % V617F before treatment . |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 26 | Imatinib | 800 mg/d | 5 | NR | 44 | ND |
| 2 | F | 60 | Imatinib | 700 mg/d | 5 | PR | 41 | 34 |
| 3 | M | 49 | Imatinib | 800 mg/d | 9 | NR | 89 | 71 |
| 4 | F | 67 | Imatinib | 500 mg/d | 9 | PR | 91 | 88 |
| 5 | M | 58 | Imatinib | 400 mg/d | 10 | PR | 72 | ND |
| 6 | M | 48 | Imatinib | 800 mg/d | 15 | PR | 57 | 40 |
| 7 | M | 31 | Imatinib | 800 mg/d | 17 | PR | 76 | 63 |
| 8 | F | 48 | Imatinib | 500 mg/d | 17 | CR | 8 | 25 |
| 9 | F | 28 | Imatinib | 800 mg/d | 19 | PR | 83 | 82 |
| 10 | M | 72 | Imatinib | 400 mg/d | 21 | NR | 72 | ND |
| 11 | M | 54 | Imatinib | 300 mg/d | 24 | CR | 21 | 44 |
| 12 | M | 43 | Imatinib | 400 mg/d | 25 | PR | 60 | 40 |
| 13 | M | 30 | Imatinib | 600 mg/d | 25 | PR | 19 | |
| 14 | M | 53 | Imatinib | 700 mg/d | 31 | PR | 30 | ND |
| 15 | F | 32 | rIFNα | 3 MU 3 times/wk | 13 | CR | 19 | ND |
| 16 | F | 39 | rIFNα | 3 MU 5 days/wk | 45 | CR | 39 | ND |
| 17 | M | 53 | rIFNα | 3 MU/day | 50 | CR | 29 | ND |
| 18 | F | 48 | rIFNα | 4 MU, alternate d | 60 | PR | 87 | ND |
| 19 | M | 42 | rIFNα | 2 MU 3 times/wk | 60 | CR | 27 | ND |
| 20 | M | 52 | rIFNα | 4.25 MU 3 times/wk | 108 | CR | 22 | ND |
| 21 | M | 39 | rIFNα | 3.5 MU/d | 132 | CR | 25 | ND |
Rx indicates treatment; F/U, follow-up (= time of sampling) after starting rIFNα or imatinib; NR, no response; ND, not determined; PR, partial response; CR, complete response; and MU, million units.
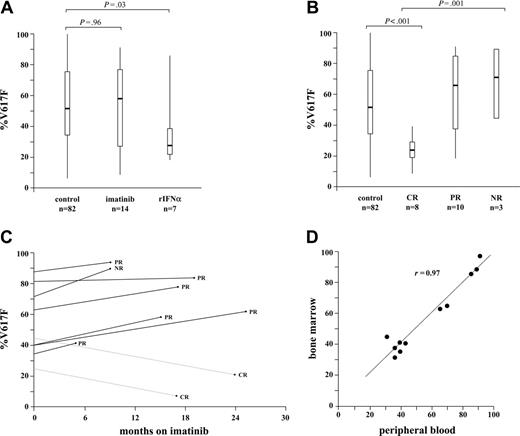
To quantify the level of disease, we used pyrosequencing, which measures the proportion of mutant alleles.17 As shown in Figure 1A, we found that the median percentage of mutated JAK2 alleles (%V617F) did not differ significantly between the imatinib-treated cases (median, 59%; range, 8%-91%) and the V617F-positive cases from the control group (median, 53%; range, 5%-100%). The %V617F was lower in the rIFNα-treated cases (median, 27%; range, 19%-87%) compared with controls (P = .03), which probably reflects the high proportion of cases in this selected group who had achieved CR rather than any preferential inhibitory effect of rIFNα over imatinib.
For imatinib-treated patients, the median %V617F for individuals with NR, PR, and CR were 72% (range, 44%-89%; n = 3), 60% (range, 30%-91%; n = 9), and 15% (range, 8%-21%; n = 2), respectively. In the rIFNα-treated group, the single case with a PR had 87% V617F compared with a median of 26% (range, 19%-39%) for the 6 cases in CR. Individuals who achieved CR on imatinib or rIFNα (n = 8) had a lower %V617F (median, 24%; range, 20%-29%) than those patients who did not achieve CR (n = 13; median, 72%; range, 19%-91%) and also the control group (P = .001). There was a significant trend in reduction of %V617F values on comparison of patients who showed NR, PR, or CR to therapy (P = .001, Figure 1B).
To determine the magnitude of any change that occurred as a consequence of therapy, we compared %V617F levels in pretreatment bone marrow and posttreatment peripheral-blood samples for 9 of the imatinib-treated cases (pretreatment samples were not available for the other cases). Of these 9 cases, the 7 with NR or PR showed a marginal increase (median, 1.2-fold; range, 1.0- to 1.5-fold) in the percentage of V617F alleles on treatment. In contrast, the 2 patients who achieved CR showed a 2- to 3-fold reduction in %V617F on treatment (Figure 1C). To confirm that these changes were not distorted by differences in the size of the V617F clone between bone marrow and peripheral blood, we compared the %V617F in contemporaneous specimens taken from 11 control PV patients. As shown on Figure 1D, similar %V617F levels are seen in blood and marrow.
Interferon-α exerts a general antimyeloproliferative effect, although its precise mechanism of action is not understood. Since pretreatment samples were not available for the rIFNα-treated cases in our study group, we cannot be certain that this therapy resulted in a reduction of %V617F levels. However, this seems likely to be the case since the rIFNα-treated patients (all but one of whom were in CR) had significantly lower %V617F levels than controls, and, furthermore, these levels were comparable with those seen in CR cases on imatinib. Indeed, subsequent to this study, we have identified a further PV patient who showed a reduction in the %V617F from a pretreatment level of 70% to 35% in CR on rIFNα.
Levels of JAK2 V617F in treated and control PV cases. (A) Comparison of %V617F in control, mutation-positive PV cases who were either treated or not treated with imatinib or rIFNα. (B) Comparison of %V617F in control PV cases and patients who showed CR, PR, or NR following therapy with imatinib or rIFNα. Vertical lines indicate the range of results; boxes, the interquartile range; and thick horizontal lines, median values. (C) Changes in %V617F on imatinib therapy. The %V617F was measured before starting imatinib and at various times while on therapy for 7 patients who showed no response (NR) or a partial response (PR), and 2 patients who showed a complete response (CR). (D) Comparison of %V617F level in peripheral blood and bone marrow from 11 control PV cases.
Levels of JAK2 V617F in treated and control PV cases. (A) Comparison of %V617F in control, mutation-positive PV cases who were either treated or not treated with imatinib or rIFNα. (B) Comparison of %V617F in control PV cases and patients who showed CR, PR, or NR following therapy with imatinib or rIFNα. Vertical lines indicate the range of results; boxes, the interquartile range; and thick horizontal lines, median values. (C) Changes in %V617F on imatinib therapy. The %V617F was measured before starting imatinib and at various times while on therapy for 7 patients who showed no response (NR) or a partial response (PR), and 2 patients who showed a complete response (CR). (D) Comparison of %V617F level in peripheral blood and bone marrow from 11 control PV cases.
Imatinib is a selective inhibitor of ABL, PDGFR, KIT, and FMS tyrosine kinases but is not active against JAK2. It is known that KIT signal transduction pathways are required for erythropoiesis,19,20 and it is possible that the observed clinical benefits of imatinib in PV are a consequence of KIT inhibition. Although our study demonstrates that molecular responses can be discerned in PV patients that correlate with hematologic improvement, the magnitude of these responses contrasts starkly with chronic myeloid leukemia, wherein many individuals experience a 1000-fold or greater reduction in BCR-ABL levels.21,22 While we cannot exclude the possibility that occasional PV patients might exhibit more substantial molecular responses, we conclude that the response of PV to imatinib or rIFNα is relatively modest.
Prepublished online as Blood First Edition Paper, December 13, 2005; DOI 10.1182/blood-2005-09-3917.
Supported by the Leukaemia Research Fund (UK), the Dr Mildred Scheel Stiftung, the Wessex Cancer Trust, the Cancer Research and Treatment Fund, and the European LeukemiaNet within the 6th European Community Framework Programme for Research and Technological Development.
A.V.J., K.W., C.C., S.K., and A.J.C. performed or supervised the laboratory analysis and contributed to the interpretation of results. R.T.S. provided samples from all imatinib- or interferon alpha-treated cases plus some controls, provided patient care, and contributed to the design of the study. K.Z., A.H., D.O., G.M., E.L., and A.R. contributed control patient samples and supplied essential data. N.C.P.C. designed the study and wrote the first draft of the paper. All authors commented on and contributed to the final paper.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal