Comment on Noble et al, page 4475
The paper by Noble and colleagues describes a novel population of regulatory CD8+ T cells that is generated in vitro by exposure of CD8+ T cells to the combination of IL-4 and IL-12.
In the 1970s, 2 types of CD8+ T cells were described: cytotoxic and suppressor, with the suppressor population found in the blood of patients who underwent allogeneic bone marrow transplantation (BMT) and Hodgkin lymphoma patients treated with total lymphoid irradiation.1,2 Suppressor T cells inhibited lectin-induced T-cell proliferation and B-cell immunoglobulin synthesis and T-cell proliferation in mixed lymphocyte reactions.3 Suppressor T cells were hypothesized to be responsible for the clinical immunosuppression observed among these patients,4 but their precise identity, distinction from effector CD8+ T cells, and mechanism of action were unclear. Interest in suppressor CD8+ T cells waned during the decades in which antigen-specific cytotoxic CD8+ T-cell responses were defined and antigen presentation by dendritic cells was discovered.
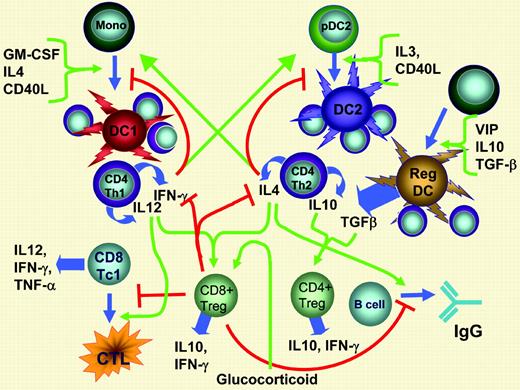
Data presented by Noble and colleagues in this issue of Blood shed new light on these interesting regulatory cells. The authors found that CD8+ Tregs inhibited the generation of Th1/Tc1 and Th2/Tc1 antigen-specific effector responses. The cytokine profile of the CD8+ Tregs was similar to that of their CD4+ counterparts, with synthesis and secretion of high levels of IL-10 and IFN-γ, but the former cells are augmented by the presence of glucocorticoids, while CD4+ Tregs were not. The presence of a phenotypically similar population following in vivo immunization suggests that this phenomenon is part of the physiologic regulation of immune responses. The data presented by the authors use OT-1 and OT-2 transgenic T cells to track antigen-specific immune responses in vivo as well as a parenteral → F1 graft-versus-host disease (GVHD) model to demonstrate physiologic relevance of the CD8 Tregs to regulating immune responses. Inhibition of antigen-specific effector immune responses required relatively high ratios of CD8+ Tregs to effectors with cell-to-cell contact, and was not blocked by neutralizing secreted IL-10 or TGF-β, or the presence of a Golgi poison to block cytokine secretion, but could be reversed by anti-CD28 antibodies. These new data indicate that the regulation of immune responses is redundant, with multiple stimulatory and inhibitory pathways that converge on the same intermediates and effector cell populations. The addition of CD8+ Tregs to the regulatory dendritic cells that are generated by TGF-β, IL-10, or VIP5 adds another important counterregulatory system that limits immune responses. The map of these connections begins to look like a New York City subway map, with overlapping routes delivering counterbalancing activation and inhibitory signals (see figure).FIG1
Pathways of immune regulation. Positive signals for immune activation are shown as green arrows; inhibitory signals are shown as red lines terminating in red bars. Blue arrows represent differentiation pathways and/or secreted cytokines. Generation of CD8+ Tregs occurs under the influence of IL-12 made by Th1 and IL-4 made by Th2 T cells.
Pathways of immune regulation. Positive signals for immune activation are shown as green arrows; inhibitory signals are shown as red lines terminating in red bars. Blue arrows represent differentiation pathways and/or secreted cytokines. Generation of CD8+ Tregs occurs under the influence of IL-12 made by Th1 and IL-4 made by Th2 T cells.
The paper by Noble et al generates many questions regarding the role of Tregs in regulating normal adaptive and pathologic immune responses. Does the generation of Tregs depend upon the initial generation of antigen-specific CD4+ T cells that release IL-4 and IL-12 into the local microenvironment? Do IL-4 or IL-12 knock-out mice have fewer CD8 Tregs in vivo and a greater propensity for dysregulated cellular immune responses, or does the redundancy of the proposed model limit the phenotype of a deficit in any single pathway? Is the toxicity of the anti-CD28 antibody recently tested in a phase 1 clinical trial due to a reversal of the inhibitory activity of Tregs? The emerging picture of immune regulation is ever more exciting in this “best of times” for immunology. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal