Comment on Martel et al, page 2710
Martel and colleagues report their meta-analysis of thromboprophylaxis studies comparing the frequency of heparin-induced thrombocytopenia (HIT) between patient groups receiving unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH). Their study supports the view that HIT is a preventable disease.
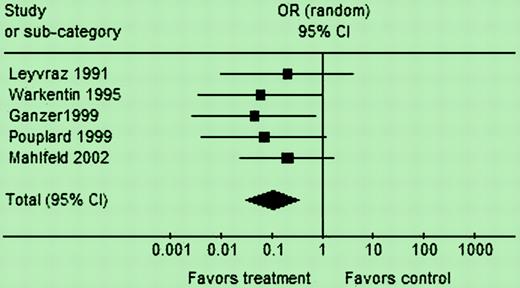
Martel and colleagues identified 5 eligible studies evaluating HIT, and an additional 10 studies measuring thrombocytopenia but not HIT. A strength of their study is that the definition of HIT required positive testing for HIT antibodies in a thrombocytopenic patient. They found the frequency of HIT to be about 10-fold less with LMWH compared with UFH (OR = 0.10 [95% confidence interval (95% CI), 0.03-0.33]; P < .001; see figure). Thrombocytopenia overall was reduced about 2-fold by LMWH (OR = 0.47 [95% CI, 0.22-1.02]; P = .06). This lower impact of LMWH upon thrombocytopenia, compared with HIT, likely reflects the inclusion of patients with non-HIT thrombocytopenia, in which influences of heparin type likely are minor.
In this same issue of Blood, Greinacher and colleagues2 provide further data in line with this meta-analysis. Notably, in this single-institution study of postorthopedic surgery thromboprophylaxis (providing further information regarding 1 of the studies3 in the meta-analysis), the lower risk of HIT with LMWH was responsible for a significant overall reduction in symptomatic thrombosis (both HIT and non-HIT) in patients receiving LMWH compared with UFH:3.9% versus 0.7% (P = .028).
Martel and colleagues point out that the impact of LMWH on reducing frequency of HIT is shown most convincingly for orthopedic surgery patients, a patient population that comprised 4 of the 5 studies in their meta-analysis that evaluated HIT as an outcome. Recently, the 7th ACCP Conference on Antithrombotic and Thrombolytic Therapy regarded the greater risk of HIT as a reason to recommend against the use of UFH for thromboprophylaxis in postorthopedic surgery patients.1 An important issue is whether the reduced risk of HIT with LMWH extends beyond postorthopedic surgery thromboprophylaxis, and can be generalized to other patient populations. This seems likely, based on a French study4 that estimated an overall 40-fold reduction in frequency of HIT with LMWH, based upon an analysis of the “numerator” of HIT cases attributed to either UFH or LMWH, and the corresponding “denominator” of estimated use of these 2 heparin preparations. Thus, HIT (and associated thrombosis) can be regarded as a preventable disease, by selection of less HIT-inducing LMWH and related compounds (fondaparinux, danaparoid) for otherwise appropriate patients. Ideally, further studies evaluating differences in risk of HIT (or its surrogate marker, platelet-activating, antiplatelet factor 4/heparin antibodies) between UFH and LMWH in different clinical settings should be performed. It is tempting to contemplate UFH perhaps someday joining ticlopidine as a “historical relic” as both become supplanted by their safer counterparts (LMWH and clopidogrel, respectively). Nevertheless, as there are certain situations (cardiopulmonary by-pass, vascular surgery, hemodialysis) in which the shorter half-life of UFH and its neutralization by protamine offer major advantages over LMWH, and because HIT sometimes occurs with LMWH (0.2% frequency estimated by Martel and colleagues), it seems that the preventable disease, HIT, will further decline—but not disappear—in the foreseeable future.FIG1
Analysis 2: HIT outcome (studies from categories A and B). See the complete figure in the article beginning on page 2710.
Analysis 2: HIT outcome (studies from categories A and B). See the complete figure in the article beginning on page 2710.
The author has declared a financial interest in a company whose product was discussed in the present work. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal