Abstract
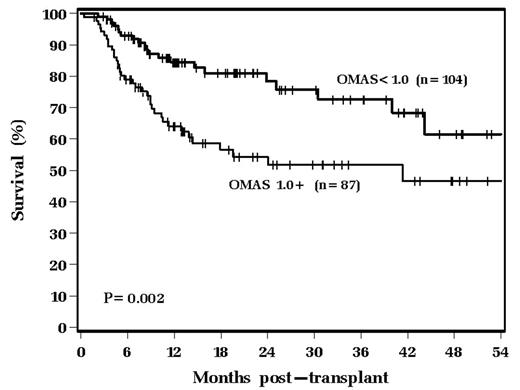
Mucositis is a well known short term complication of ABMT. Many studies of mucositis in ABMT, however, are flawed due to heterogeneity of both mobilizing regimens and high-dose preparative regimens. There is also sparse data on the long term consequences of mucositis after ABMT. This study retrospectively reviews all patients with lymphoid malignancies undergoing ABMT from 5/2000 to 2/2005 at our institution that received a uniform mobilizing regimen of VP-16 plus G-CSF and a uniform high dose preparative regimen of busulfan, cyclophosphamide and VP-16. 191 patients fit the entry criteria into this study. Mucositis was graded using the OMAS mucositis grading scale, which has a scoring range of 0–2.0. Severe mucositis for the purposes of this study was designated as having a maximal OMAS scale of ≥ 1.0. 87 patients experienced severe mucositis and 104 did not. Median age for patients was 52 years; underlying diagnoses were non-Hodgkin’s Lymphoma (n=155) and Hodgkin’s Disease (n=36). The two groups (developing severe mucositis vs not) were balanced with respect to disease status at transplant, number of courses of prior chemotherapy, prior exposure to radiation therapy of any kind, and elevated LDH at the time of transplant. Median CD34+ cell dose collected for the entire group was 8.5 x 106 /kg; there was no difference between the 2 groups. Severe mucositis correlated with mortality within 100 days of transplant. Patients with a maximal OMAS scale of < 1.0 had 99% 100-day survival (103/104) as compared to 92% (80/87) for those with an OMAS scale ≥ 1.0 (p=0.015). To date, 30% of patients have relapsed with no difference in the two groups. However, Kaplan-Meier estimates of survival reveal that severe mucositis has a profound negative impact on survival (p=0.002) as shown graphically below:
One of the key drivers of this difference in survival was the fact the patients with severe mucositis were more likely to experience pulmonary or multi-organ failure as a cause of death: 8 patients with severe mucositis died of these toxicities, as compared to zero in the less severe mucositis group. Multivariable Cox analysis was performed to analyze risk factors for mortality. Three variables were found to be significant: elevated LDH at transplant (p=0.03), number of prior chemotherapy regimens (for one regimen increase, p=0.024) and severe mucositis (p=0.003). In conclusion, patients that develop severe mucositis have a higher risk of mortality after ABMT. The etiology is likely multi-factorial; mucositis may directly contribute to mortality risk, and may also be a surrogate marker of other organ toxicities.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal