Abstract
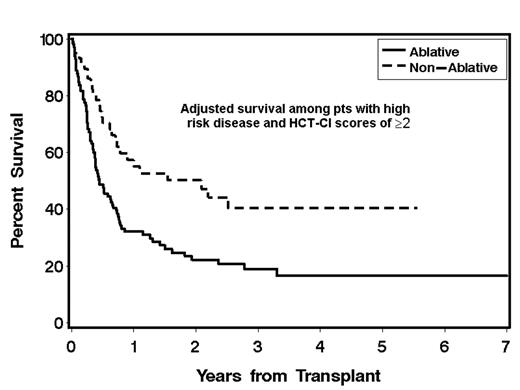
We developed a new HCT-specific comorbidity index (HCT-CI) as a sensitive tool to capture pretransplant comorbidties among pts given allogeneic HCT (Sorror et al, online, 2005; DOI 10.1182/blood-2005-05-2004). In the current report, we used the HCT-CI to explore differences in the tolerability of nonablative compared to ablative HCT in MDS or AML pts with pretransplant comorbidities. Consecutive pts (n=88) receiving nonablative conditioning with 2 Gy total body irradiation (TBI) alone (6%) or with 90 mg/kg of fludarabine (94%) were compared to concurrent pts (n=361) conditioned with cyclophosphamide plus busulfan (70%) or 12–14 Gy TBI (30%). All pts were classified into low (AML-first complete remission or MDS-refractory anemia) and high-risk disease (all others). Overall, 76% of nonablative pts had AML compared to 66% of ablative pts. At HCT, nonablative pts differed substantially from ablative pts with respect to age (median 60 vs 46 years), use of unrelated donor grafts (57% vs 42%), use of marrow grafts (5% vs 20%), and HCT-CI scores of ≥2 (75% vs 45%). Smaller differences existed for high-risk disease (64% vs 58%) and pt cytomegalovirus positive sero-status (59% vs 55%). Proportional hazards models were used to estimate the hazard ratio (HR) for non-relapse mortality (NRM) and survival for pts receiving nonablative compared to ablative conditioning regimens; these models were adjusted for stem cell source, pt age, donor type, pt cytomegalovirus sero-status, diagnoses (MDS vs AML), and HCT-CI scores (Table). Adjusted HRs were not statistically significantly different, except among pts with high-risk disease and HCT-CI scores of ≥2 where nonablative pts had lower HR for NRM (0.34, P=0.005) and worse survival (0.51, P=0.006, Fig.1). These results suggest that pts with high-risk MDS or AML and HCT-CI scores of ≥2 might have less NRM and better survival with nonablative than with ablative HCT. Prospective randomized trials are warranted to confirm this retrospective observation. Additional data are needed for AML and MDS pts with low comorbidities or low disease risk in order to clarify the usefulness of nonmyeloablative conditioning.
Adjusted hazard ratios for pts receiving nonablative relative to ablative conditioning
| . | Nonablative/ablative . | NRM . | Survival . | ||
|---|---|---|---|---|---|
| . | Number . | HR* (95% CI) . | P . | HR* (95% CI) . | P . |
| *HR <1 indicates more favorable outcome for pts receiving nonablative conditioning | |||||
| Low-risk disease | |||||
| HCT-CI scores 0–1 | 7/86 | 0.0 (undefined) | 0.33 | 0.8 (0.1–6.3) | 0.83 |
| HCT-CI scores ≥2 | 25/64 | 1.97 (0.7–5.9) | 0.23 | 1.86 (0.8–4.1) | 0.13 |
| High-risk disease | |||||
| HCT-CI scores 0-1 | 15/112 | 0.60 (0.1–2.7) | 0.51 | 0.96 (0.5–2.0) | 0.92 |
| HCT-CI scores ≥2 | 41/99 | 0.34 (0.2–0.7) | 0.005 | 0.51 (0.3–0.8) | 0.006 |
| . | Nonablative/ablative . | NRM . | Survival . | ||
|---|---|---|---|---|---|
| . | Number . | HR* (95% CI) . | P . | HR* (95% CI) . | P . |
| *HR <1 indicates more favorable outcome for pts receiving nonablative conditioning | |||||
| Low-risk disease | |||||
| HCT-CI scores 0–1 | 7/86 | 0.0 (undefined) | 0.33 | 0.8 (0.1–6.3) | 0.83 |
| HCT-CI scores ≥2 | 25/64 | 1.97 (0.7–5.9) | 0.23 | 1.86 (0.8–4.1) | 0.13 |
| High-risk disease | |||||
| HCT-CI scores 0-1 | 15/112 | 0.60 (0.1–2.7) | 0.51 | 0.96 (0.5–2.0) | 0.92 |
| HCT-CI scores ≥2 | 41/99 | 0.34 (0.2–0.7) | 0.005 | 0.51 (0.3–0.8) | 0.006 |
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal