Abstract
<Background> Previous reports about comparison between unrelated donor and cord blood for acute leukemia with myeloablative regimens showed that at least relapse rate (RR) and overall survival (OS) were not significantly different in the two groups. However we have not yet understood comparison among R-PBSCT, U-BMT, and U-CBT with reduced intensity regimens for elderly AML/MDS patients.
<Objective> The 1st purpose of this report was to investigate OS and causes of death and the 2nd was to investigate engraftment, incidence of acute/chronic GVHD, and RR for AML/MDS patients received R-PBSCT, U-BMT, and U-CBT with reduced intensity regimens.
<Patients/Methods> We reviewed medical records of 62 AML/MDS patients who had received RIST between June 2001 and March 2005 at Toranomon Hospital, Tokyo, Japan. 20 patients received R-PBSCT, 19 patients U-BMT, and 23 patients U-CBT. Median age was 56 years (17–70). Primary diseases were de novo AML (n=34) and MDS overt leukemia (n=11), and MDS (n=17) including advanced (n=47) or standard (n=15). Median follow-up was 7.2 months (1.5–37). Conditioning regimen consisted of Fludarabine (Flu) + Busulfan (BU) with cyclosporine (CyA) + MTX in R-PBSCT, Flu + BU + TBI 4Gy with CyA or tacrolimus +MTX in U-BMT, and Flu + Melphalane (Mel) + TBI 4Gy with tacrolimus only in U-CBT, respectively. G-CSF was used after RIST until neutrophile engraftment.
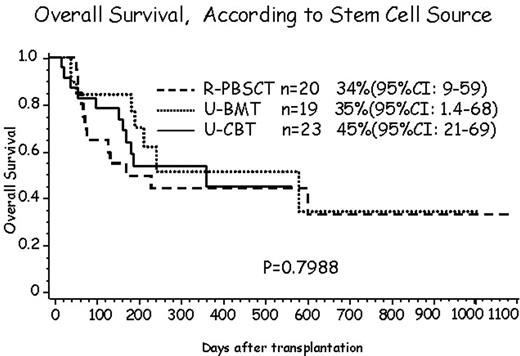
<Results> HLA disparities were 6/6 match (n=18) and 5/6 (n=2) in R-PBSCT, 6/6 (n=18) and 5/6 (n=1) in U-BMT, and 5/6 (n=2) and 4/6 (n=21) in U-CBT, respectively (P<0.001) and infused CD34 cell counts were 3.6, 1.53, and 0.081 ×10E6/kg, respectively (P<0.001). Neutrophile (>500/μL)/platelet recovery (>20,000/μL) were observed 100% (median 16.5 days) and 90% (13.5) in R-PBSCT, 90% (20) and 79% (26) in U-BMT, and 91% (21.5) and 70% (41.5) in U-CBT, respectively (P<0.05). In R-PBSCT, U-BMT, and U-CBT cumulative incidence of acute GVHD (II-IV) was 50%, 59% and 30%, and chronic GVHD was 30%, 29%, and 25%, respectively (NS). Causes of death included infections (n=5), GVHD (n=8), TRM (n=1) and progressive disease (n=16) in total cases after RIST and there was no difference among three groups. OS was 43% (95% CI: 26–59) in all cases, 69% (95% CI: 26–59) in standard, and 39% (95% CI: 24–54) in advanced, respectively (p<0.05). According to stem cell sources, OS and RR was 64%, 34% in R-PBSCT, 68%, 35% in U-BMT, and 59%, 45% in U-CBT, respectively (NS).
<Discussion/Conclusion > In this report, the differences were followings; HLA disparities, infused CD34 cell dose, conditioning regimen with GVHD prophylaxis, neutorphile and platelet engraftment. The incidence of acute/chronic GVHD, OS, RR, and causes of death were same among three groups. This Flu+Mel+TBI 4Gy + tacrolimus with U-CBT would be feasible and acceptable for elderly patients with AML/MDS.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal