Abstract
Introduction: Although allogeneic hematopoietic stem cell transpslantation is the only curative treatment for patients with MF, the potential role of cord blood transplantation remains still unclear. We report the results of RICBT for hematological diseases with primary and secondary MF.
Patients and Methods: We reviewed medical records of 179 patients with advanced hematological diseases who received RICBT between March 2002 and June 2005 at our institution. Of 179 patients, pre-transplant bone marrow specimens were available for 82 patients. We evaluated bone marrow specimens by aspiration and trephine biopsy. Aspiration may be not enough to evaluate marrow fibrosis, but could reflect fibrotic change in bone marrow (
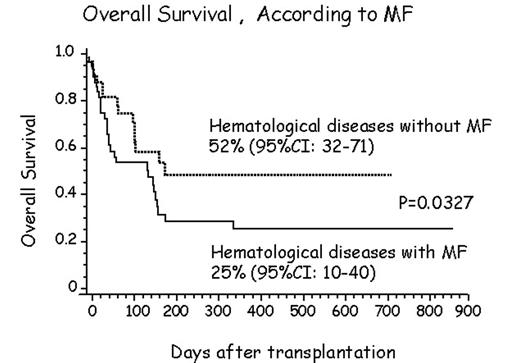
Results: Neutrophil engraftment at day 50 was observed in 70.8 % with MF (median 22 days) and 73.7 % without MF (median 22 days). Platelet engraftment at day 100 was observed in 40.0 % with MF (median 42 days) and 60.0 % without MF (median 40 days). There was no statistical significance in neutrophil and platelet engraftment between patients with MF and without MF. Of 48 patients, 6 showed biopsy-proven MF greater than stage 1. Their neutophil and platelet engraftment was observed in 100 % (median 22 days) and 66.7 % (median 48 days), respectively. Cumulative incidence of acute GVHD (II–IV) was 17 % with MF and 28 % without MF. There was no statistical significance. The estimated OS was 25 % with MF and 52 % without MF (p=0.03) (Figure 1). Most cause of death with MF was relapse.
Conclusion: Despite of marrow fibrosis, neutophil and platelet engraftment was not influenced. These results have suggested that RICBT is feasible for MF. However, the existence of MF could be poor prognostic factor of RICBT for hematological diseases due to relapse.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal