Abstract
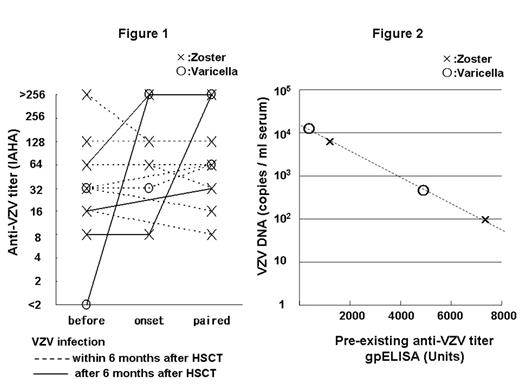
Reactivation of varicella-zoster virus (VZV) is common among recipients of hematopoietic stem cell trasnplantation (HSCT). In this setting, VZV infection can occur frequently as localized zoster (shingles) and sometimes as disseminated varicella (chickenpox) with or without visceral involvement, which results in a high mortality rate. Previous studies revealed that VZV-specific memory T cells play a crucial role in suppressing reactivation. Although varicella zoster immunoglobulin is used as a prophylactic and treatment modality in some contries, the role of humoral immunity against VZV infection has been poorly evaluated. The aim of the study was to identify the relationship between quantitative transition of VZV antibody titers and clinical manifestation of VZV infection in HSCT recipients. Thirteen patients with VZV infection after HSCT (7 males, 6 females; age: 21–65 years, median age: 35 years) were enrolled. Eleven patients (allo, 7; auto, 4) suffered localized zoster. Two patients (both allo) suffered systemic varicella with visceral involvement (1 with acute abdomen and 1 with interstitial pneumonia). All patients were treated with acyclovir. Seven patients who had been followed for at least 3 years after HSCT without clinical VZV infection were studied as control subjects (4 males, 3 females; age: 16–40 years, median age: 28 years; allo, 6; auto, 1). We retrospectively studied transition of anti-VZV-IgG titer by the IAHA and gpELISA method (before and at 3, 6, 12, 24, 36 months after HSCT) and VZV-DNA by realtime PCR during clinical VZV infection (onset and paired serum) using cryopreserved serum samples. All patients were seropositive for VZV before HSCT. One of the patients (the most severe case) had become seronegative before systemic varicella developed. However, VZV infections in the other 12 patients occurred despite the persistent existence of anti-VZV (IAHA:x8 to >x256; median x32). There are no statistically significant differences between anti-VZV titers in the 13 patients with VZV infection and those in the 7 controls at each time point. Acceleration of the titer (>x4) was not observed in any of the 9 recipients with VZV infection within the first 6 months after HSCT but was observed in 3 of 4 recipients with VZV infection after 6 months (Figure 1). Four available samples at onset of VZV infection (varicella, 2; zoster, 2) were all positive for VZV-DNA (94.4 to 12173.3 copies /ml serum) by realtime PCR, whereas VZV was undetectable in all paired sera (2 to 5 weeks after onset). Pre-existing anti-VZV titer (gpELISA) and serum viral load were inversely correlated (Figure 2). In HSCT recipients, pre-existing antibody does not prevent development of VZV reactivation but may contribute to decreased viral load, resulting in a mild clinical course. Despite the localized clinical feature of zoster, VZV was detected in serum samples from zoster patients. Clinicians should be aware of the risk of airborne transmission of VZV from HSCT recipients with either varicella or zoster.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal