Abstract
In EORTC-LCG AML-10 study patients with low CD34 mobilization profile showed a better outcome (Leukemia,2003,17:60-7). We hypothesized that patients with low pCD34 at the recovery period after RI therapy with de novo AML should have a better clinical outcome or vice versa and launched this prospective study. Between Jan 2002 and Oct 2004, 40 patients with AML (median age: 40 yrs, 17–60; 22M/18F) were enrolled to this study. Using flow cytometrical method CD34-expressing cells were measured in peripheral venous blood samples once WBC was between 1x10e9/L to 3x10e9/L at the recovery period after first RI therapy.
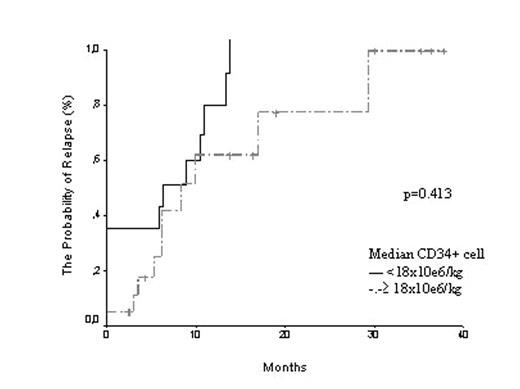
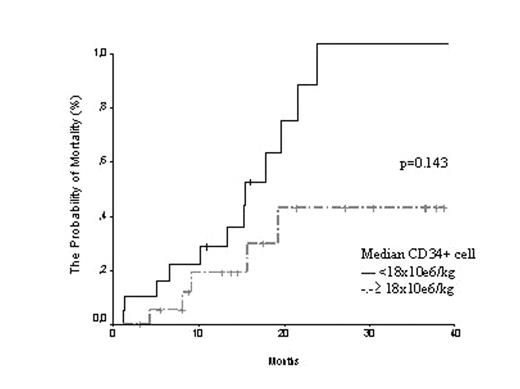
Results: The median time for estimation of pCD34 was 23 days (7–35) after RI. The pCD34 cell count was lower in patients responding to first RI therapy (12x10e6/L vs 68x10e6/L, p=0.011). We observed a weak, but statistically significant positive correlation between CD34 expression of the blasts at diagnosis and pCD34 at recovery period (p=0.048, r2:0.322). We could not show any significant negative impact of CD34 expression of the blasts at diagnosis and response to first RI (p=0.059). Only two of 8 patients not responding to the 1st RI achieved a complete remission after re-induction. The two-year probability of OS, LFS, relapse incidence and mortality rates were 47.1%, 37.2%, 55% and 42.5%, respectively (fig 1,2). If we set up a cut-off value of 18x10e6/L for pCD34, we did not observe any impact of pCD34 on relapse incidence but the mortality rate was significantly increased in patients with high CD34+ cell count (p=0.025).
Conclusion: We were able to show a positive impact of pCD34 estimations after first RI in AML patients on both remission and mortality rate. AML Patients with lower pCD34 after 1st RI tends to have a higher hematological remission rate and lower mortality. This impact of pCD34 as a predictive and prognostic marker in AML should be verified in large cohorts using multivariate analysis.
Distribution of risk factors at diagnosis according RI response
| Variables . | 1stCRafter1stRI (n=32 ) . | NoCR after 1stRI (n=8 ) . | P . |
|---|---|---|---|
| *p<0.05; Abbr: NS: Non-Significant; ND: Not-Done | |||
| pCD34 (x10e6/L) | 12.4 (0–268) | 68.6 (4.4–3820) | 0.011* |
| CD34 expr at dx | 12% (0%–94%) | 44% (9–89) | 0.059 |
| Age, years | 38.5 (17–57) | 43 (20–60) | NS |
| WBC at dx (x10e9/L) | 11.85 (0.7–175.0) | 5.10 (2.7–114.7) | 0.934 |
| EM involvement (Y/N) | 7/25 | 0/8 | NS |
| Variables . | 1stCRafter1stRI (n=32 ) . | NoCR after 1stRI (n=8 ) . | P . |
|---|---|---|---|
| *p<0.05; Abbr: NS: Non-Significant; ND: Not-Done | |||
| pCD34 (x10e6/L) | 12.4 (0–268) | 68.6 (4.4–3820) | 0.011* |
| CD34 expr at dx | 12% (0%–94%) | 44% (9–89) | 0.059 |
| Age, years | 38.5 (17–57) | 43 (20–60) | NS |
| WBC at dx (x10e9/L) | 11.85 (0.7–175.0) | 5.10 (2.7–114.7) | 0.934 |
| EM involvement (Y/N) | 7/25 | 0/8 | NS |
The outcome of AML patients according to median pCD34 at recovery
| Variables . | pCD34<Med 18x10e6/kg (n=20 ) . | pCD34 ≥ Med 18x10.6/kg (n=20) . | p . |
|---|---|---|---|
| CR1 (Y/N) after 1st RI | 19/1 | 13/7 | 0.044* |
| Relapse incidence | 44% | 54.5% | NS |
| Mortality rate | 25% | 60% | 0.025* |
| DFS | 46.19%±12.6% | 29.2%±10.4 | NS |
| OS | 64.95%±13.2% | 35.6%±11.3 | NS |
| Variables . | pCD34<Med 18x10e6/kg (n=20 ) . | pCD34 ≥ Med 18x10.6/kg (n=20) . | p . |
|---|---|---|---|
| CR1 (Y/N) after 1st RI | 19/1 | 13/7 | 0.044* |
| Relapse incidence | 44% | 54.5% | NS |
| Mortality rate | 25% | 60% | 0.025* |
| DFS | 46.19%±12.6% | 29.2%±10.4 | NS |
| OS | 64.95%±13.2% | 35.6%±11.3 | NS |
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal