Abstract
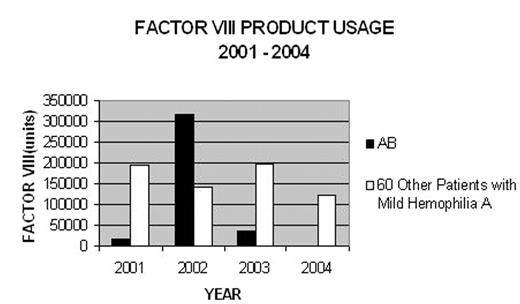
AB is a 73 year old Caucasian male who was diagnosed with mild Hemophilia A in 2001. He is part of a large kindred of patients with mild Hemophilia A enrolled in a cohort study. His family history was strongly positive. He was referred at the age of 69 years by a family member. His baseline Factor VIII level was 0.10. AB’s past medical history is characteristic of mild Hemophilia A. As a child he suffered frequently from epistaxis. He bled extensively after lacerations. He had had three significant accidents during his adult years, each of which resulted in massive bleeding and multiple blood transfusions. He had had three dental extractions which resulted in significant bleeding during two of three procedures. He had a hydrocele repair without complications. In 1999, he was extensively investigated for melena with no cause. He had an episode of atrial fibrillation and a possible transient ischemic attack treated with warfarin and aspirin. AB reported significant joint swelling and decreased range of motion. He also reported that he had “a leaky heart valve’. His initial physical examination revealed significant musculoskeletal problems. He had decreased range of motion bilaterally in his hips. He had extensive swelling of both knees and decreased range motion of both ankles. There was a limb length discrepancy of 1.5 cm. AB denied severe joint pain in his lower limbs or the usual symptoms associated with hemophiliac arthropathy. His aPTT was prolonged but he had not had a Factor VIII level previously measured and had never been told that he had Hemophilia A. He received a trial of prophylactic Recombinant Factor VIII three times a week for two months and was referred to an orthopedic surgeon. He received a “Factor First” Identification card recommending he receive 4000 units Recombinant Factor VIII for a major bleed. However, he had great difficulty in accepting the diagnosis and neither he nor his family initially volunteered that he had Hemophilia on his next admission. In April, 2002, AB was admitted to ICU in a community hospital, in Diabetic Ketoacidosis, three weeks after a snowmobile accident. Retrospectively, he reported back pain which he managed with NSAIDS. He was unable to walk prior to his hospitalization. In ICU, he required daily transfusions of PRBC & FFP. Abdominal CT on admission reported a resolving iliopsoas hematomas after an upper gastrointestinal bleed he was transferred to the provincial tertiary care centre. Follow-up CT showed bilateral ilopsoas hemtomas with abscess formation. A CT guided aspiration confirmed the presence of Staphyloccus aureus and a left paravertebral abscess. Follow-up CT showed no improvement. A second CT guided aspiration was performed which showed vertebral body destruction of L3, L4 and L5, discitis and multiple abscess formation. AB underwent L3-S1 fusion with laminectomy and decompression of L3–L4 and L4–L5 with no complications. In total AB received 316,040 units of RF VIII during a 122 day period of hospitalization. In contrast, the other 60 patients enrolled in our study only used 656,515 in a 4-year period.
FACTOR VIII PRODUCT USAGE 2001–2004
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal