Abstract
Objectives. Sickle cell disease (SCD) is the most common single gene disorder in black Americans, with poorly described cardiovascular sequelae partly due to insensitive techniques to identify microvascular perfusion abnormalities. We employed cardiac magnetic resonance (CMR) and computed tomography (CTA) to assess myocardium, microvascular perfusion and coronary arteries in SCD patients.
Methods. Twelve adult patients with SCD (10 HbSS, 1 HbSC and 1 S-thal) age 20–45 years were enrolled. CMR protocol included: dark blood multiecho imaging, rest and stress myocardial perfusion, multiplane cines, and delayed post-gadolinium imaging (DME) for infarct imaging. Myocardial T2*, reflecting iron content, was calculated and verified using a T2* phantom. Left and right ventricular volumes and ejection fractions were quantified from short axis cines. Coronary CTA was performed in patients and five controls using a 64-slice scanner and 70cc of isotonic, isoosmolar contrast, with vessel review in multiple planes.
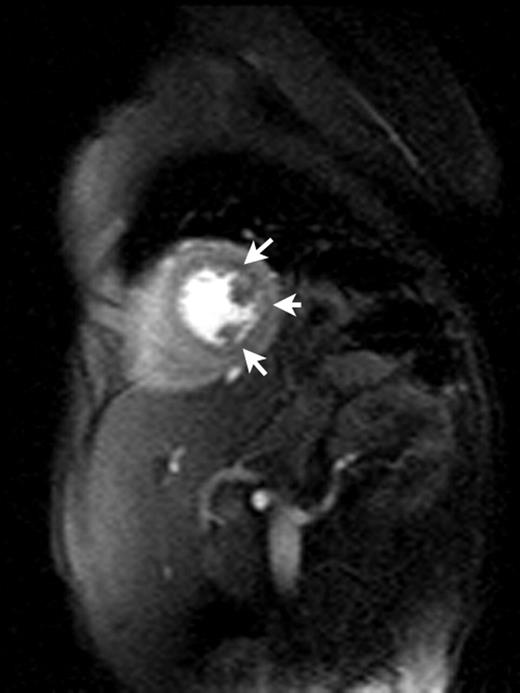
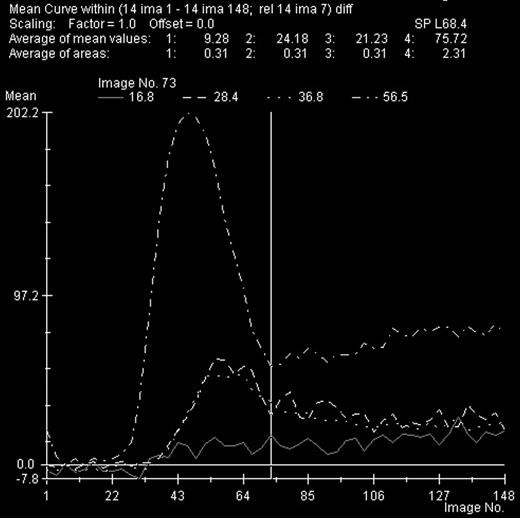
Results. Three subjects, all SS genotype, had striking subendocardial ischemia (top image, arrows) with vasodilator stress that was not present at rest (signal intensity-vs-time curves, solid line=abnormal subendocardium, dotted and dashed=normal myocardium, dot-dash=blood pool). Myocardial T2* was normal in all subjects (25 to 33ms) as were DME, LV mass and LVEF. One subject with pulmonary hypertension had marked RV dysfunction (RVEF 26%). No subject had obstructive epicardial coronary disease, though proximal coronary diameters were significantly larger for SCD patients compared to controls (2.7mm/m2 versus 1.9mm/m2, p<0.001).
Conclusions. A subset of SCD patients has quantifiable myocardial ischemia with coronary dilatation and absence of infarcted myocardium. Further studies are ongoing to correlate perfusion abnormalities with episodic chest pain and ischemia-based therapies.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal