Abstract
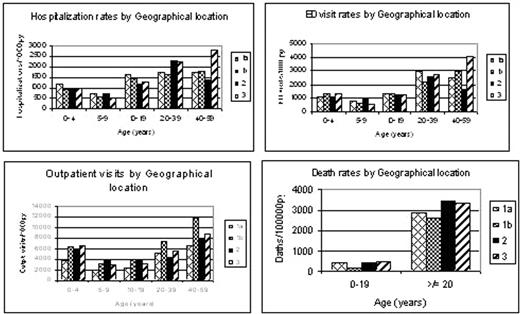
The mortality of children less than 5 years of age with SCD has decreased substantially and now is similar to that of children without SCD. However the impact of comprehensive care on health outcomes of SCD has not been fully evaluated. This study compared the medical care utilization and mortality in children and adults with SCD in four regions in the state of Tennessee with variable access to a comprehensive sickle cell center (CSCC). This is a retrospective longitudinal study of a cohort of patients with SCD enrolled in TennCare, Tennessee’s Medicaid managed health care program, from January 1995 to December 2002. Children and adults who had at least one inpatient or two outpatient physician visit claims, at least 30 days apart, listing an International Classification of Diseases, Ninth Revision, Clinical Modification code for SCD (homozygous, SC, sickle beta thalassemia) constituted the cohort. TennCare data linked to Tennessee vital records were used to define the population and identify the outcomes. One of the four large urban counties in Tennessee has a CSCC. The patients were assigned to one of four regions based on the area of residence on the day of their hospitalization or outpatient visit: Area 1a- urban county where CSCC is located, Area 1b- counties surrounding the CSCC area, Area 2: 3 urban counties which include large academic medical centers, Area 3- the remainder of Tennessee counties. Rates of hospitalizations, outpatient and emergency department (ED) visits, and deaths were compared in the four regions of the state. The cohort included 2102 patients with a total of 11,814 person-years (py). 58% of patients resided in area 1a, 9% in area1b, 19% in area 2 and 14% in area 3. 59% were females and 49% were older than 20 years. 14% were younger than 5 years. The following figure shows the rates of hospitalizations, ED and outpatient visits and deaths in 4 regions. Among children less than 5 years of age the rate of hospitalization was highest in area 1a (p<0.001). ED and outpatient visits for children were highest in area 3, (p<0.001). Among adults, 20 years or older, the rates of hospitalization and ED visits were highest in area 3, (p<0.001). The outpatient visits were highest in area1b (p<0.001). There was no significant difference in the death rates in the four regions. Males had significantly higher death rates in all regions (p<0.001). Trend analysis over 8 years showed a significant trend for increased rates of ED and outpatient visits in all regions (p<0.001) and deaths in area 2 (p=0.014). No clear pattern of improved outcomes as measured by hospitalizations, ED and outpatient visits and deaths are identified in relation to access to a CSCC or large academic medical centers. Area of residence may not affect care for SCD. Alternatively, there may be selective distribution of sicker patients in these areas based on their need for care.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal