Abstract
Donor-recipient histocompatibility is a major determinant of outcome after UD HSCT, and matching pairs by high-resolution (Hi-res) HLA typing is likely to improve results.
Methods: We studied 66 pts with myeloid leukemias in complete remission (CR) transplanted with UD bone marrow (n=58) or peripheral blood (n=8) from 01/02 to 12/04. Preparative regimens were ablative [Busulfan (Bu)/Cyclophosphamide (Cy)(n=13), Cy/TBI (n=2), Fludarabine (Flu)/Bu 130 mg/m2x4 doses (n=33)] and reduced intensity [Flu/Bu 130 mg/m2x2 doses+Gleevec (n=7), Flu/Melphalan 140mg/m2 (n=11)]. ATG was given in 61 cases. GVHD prophylaxis was tacrolimus and mini-methotrexate, with additional pentostatin in 24 pts. Hi-res typing of HLA-A, B, DRB1 and DQB1 loci was done prospectively; HLA-DPB1 and C loci were typed prospectively in 50% of cases and retrospectively in 50%. Hi-res typing was sequencing-based for HLA-A, B, DRB1, SSP-based for DRB3/4/5, DQB1 and DPB1; and SBT/SSOP-based for HLA-C. A Cox’s proportional hazards regression model was used to study overall (S), event-free (EFS) and aGVHD-free survival. Variables with a p-value <0.25 by univariate analysis were included in the multivariate model (MV). Variables were age, conditioning regimen, use of pentostatin, diagnosis, cytogenetics, SC source, ABO typing, infused total nucleated cell (TNC) dose, HLA matching and GVHD.
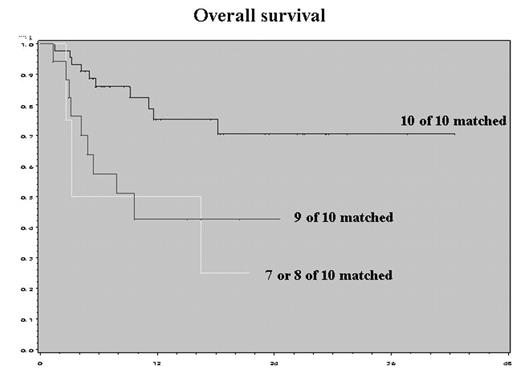
Results: Median age was 45yrs (21–72). Diagnoses were MDS (n=5), AML (n=39), and CML (n=22). 21 pts were in 1st CR, 23 pts in 2nd or 3rd CR, 22 pts in 2nd or greater chronic phase (CP) CML. 45 pts were 10/10 HLA match (HLA-A, B, C, DRB1, DQB1), and 21 had one or more mismatches. All pts engrafted neutrophils at a median of 13 days; 32 pts (48%) had gd. II–IV aGVHD and 33 pts (57%) had cGVHD. With a median follow-up of 9 mo, 44 pts are alive; 11 pts have relapsed. There were no regimen-related deaths; 100-day mortality was 13% due to aGVHD (n=7), relapse (n=1) and infection (n=1). Median S and aGVHD-free survival in 10/10 pts have not been reached. Median EFS for 10/10 pts vs others is 34 vs.9.66 mos. MV for S: age ≥60yrs (P=0.02; HR 4.17 (95%CI 1.24–14), Flu-based regimen (P=0.0004; HR 0.14 (95%CI 0.05–0.41), use of pentostatin (P=0.02; HR 0.27 (95%CI 0.09–0.78) and grade II–IV aGVHD (P=0.02; HR 3.25 (95%CI 1.19–8.88). MV for EFS: age ≥60yrs (P=0.046; HR 3.06 (95%CI 1.02–9.18), Flu-based regimen (P=0.001; HR 0.21 (95%CI 0.08–0.54) and use of pentostatin (P=0.02; HR 0.34 (95%CI 0.13–0.85). MV for aGVHD-free survival: age ≥60yrs (P=0.039; HR 3.43 (95%CI 1.06–11.1), Flu-based regimen (P=0.0027; HR 0.09 (95%CI 0.02–0.43), use of pentostatin (P=0.003; HR 0.22 (95%CI 0.08–0.6) and CP CML (P=0.004; HR 0.06 (95%CI 0.01–0.41). S and EFS for 10/10 matched pts were improved with Flu-based regimen (p=0.01), and higher infused TNC dose (p=0.02). aGVHD-free survival was improved by using reduced intensity regimens (p=0.004) and worsened by presence of 2 DPB1 mismatches (1.18 mo vs not reached; HR=3.43; p=0.08).
Conclusion: A combination of donor selection by high-resolution typing, less toxic preparative regimens and improved GVHD prophylaxis can optimize outcomes in this high-risk disease context.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal