Abstract
<Background>Allogeneic stem cell transplantation (allo-SCT) is a curative treatment for advanced myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML). The therapeutic benefits are attributable to myeloablative radiochemotherapy and graft-versus-leukemia effect, whereas severe regimen-related toxicity (RRT) limits the efficacy of allo-HSCT to young patients without co-morbidities. Reduced-intensity stem-cell transplantation (RIST) using a non-myeloablative preparative regimen has been developed to decrease RRT, whilst preserving an adequate antitumor effect. RIST may be a curative treatment for heavily pretreated elderly patients with myeloid malignancies. Umbilical cord blood from unrelated donors has been used as an alternative stem cell source. We report the results of reduced-intensity unrelated cord-blood transplantation (RI-UCBT) in patients with advanced or high-risk myeloid malignancies.
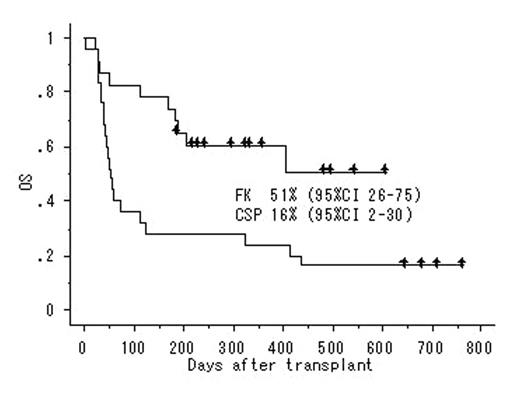
<Patients and Methods>Forty-eight patients (median age, 59 yr; range, 17–70) underwent RI-UCBT with a preparative regimen consisting of fludarabine 125 mg/m2, melphalan 80 mg/m2, and 4 Gy of total body irradiation from 2002 to 2004. Twelve-seven patients were classified as AML not otherwise categorized, 16 as AML with multilineage dysplasia, 4 as RAEB and 1 as RA. The disease status at transplant was 2 CR1, 5 CR2 or CR3, 3 untreated and 38 refractory. The median infused total cell dose was 2.8 (range, 1.8–4.5) x 107/kg. HLA match was 6/6 in 1, 4/5 in 8, and 4/6 in 39 cases. GVHD prophylaxis was composed of cyclosporine (n=25) or tacrolimus alone (n=23).
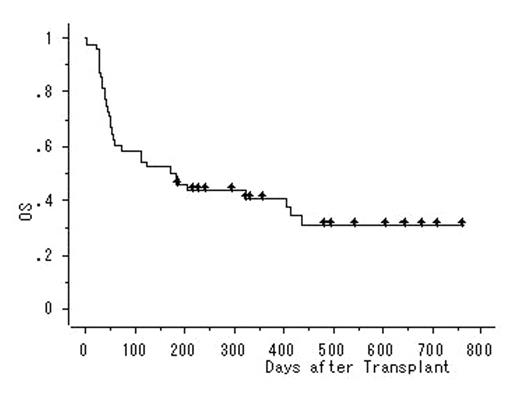
<Results> Fourty-three patients achieved primary neutrophil engraftment after a median of 20 days. Twelve patients developed grade II–IV acute GVHD and 7 developed chronic GVHD. Fifteen patients achieved CR. Eleven patients experienced relapse. Thirty-one patients died as a result of relapse (n=10), GVHD-associated complications (n=10), or infection (n=11). With a median follow-up of 489 days (range, 192–768), 17 of 48 patients are alive, resulting in a 2-year overall survival rate of 31% (95% CI, 16% to 45%). GVHD prophylaxis influenced outcomes (p<0.05).
<Discussion> These data suggest that RI-UCBT may be an effective option for patients with high-risk myeloid malignancies who lack an HLA-matched donor. RI-UCBT is associated with high TRM, providing a rationale for a larger clinical study, which should be modified to focus on enhancing any GVL effect, minimizing toxicities, and controlling infectious complications.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal