Abstract
Background. Pulmonary hypertension, defined by an elevated pulmonary artery systolic pressure measured by Doppler-echocardiogram, has been identified as the major predictor of death in the adult sickle cell disease population. While diastolic dysfunction is also observed in this population, the prevalence in unselected patients, the association with high pulmonary artery systolic pressure, and the attributable mortality remain unknown.
Methods. Diastolic function parameters, pulmonary artery systolic pressures and right and left ventricular size and function were measured prospectively in 215 subjects with sickle cell disease. Associations between these parameters, lab and echocardiographic variables and prospective mortality were determined.
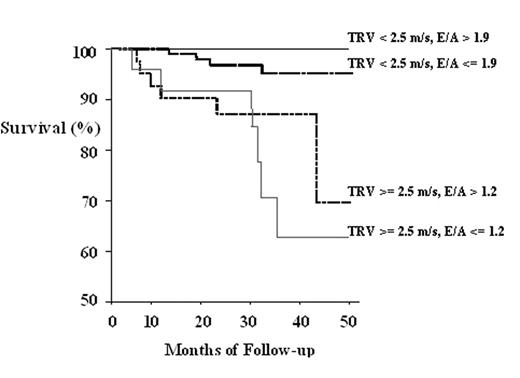
Results. Diastolic dysfunction, measured by conventional and tissue-Doppler echocardiography, was present in 19% of patients with sickle cell disease. Diastolic dysfunction and pulmonary hypertension were both present in approximately 11% of patients and diastolic dysfunction accounted for approximately 10–20% of the variability in tricuspid regurgitant jet velocity. Importantly, Cox Proportional Hazards analysis revealed that diastolic dysfunction, as reflected by low E/A ratio, was associated with prospective mortality with a risk ratio of 1.9 (95%CI 1.0 to 3.7; p=0.028), even after adjustment for tricuspid regurgitant jet velocity. While pulmonary hypertension remained the dominant determinant of mortality risk, even after adjustment for measures of diastolic function (adjusted rate ratio of 5.3; 95% CI= 1.9 to15.0; p<0.001), the risk was additive such that patients with both risk factors had an odds ratio for death of 10.1 (95% CI= 3.2 to 31.9; p<0.001).
Conclusions. Diastolic dysfunction and pulmonary hypertension due to other causes each contribute independently to prospective mortality in patients with sickle cell disease. Patients with both risk factors have an extremely poor prognosis. These data support the implementation of Doppler-echocardiographic screening of adult patients with sickle cell disease to identify individuals at high risk of death for intensified therapy.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal