Abstract
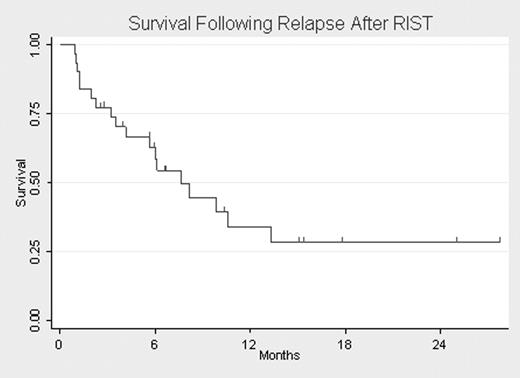
Patients (pts) with leukemia who relapse after myeloablative allogeneic stem cell transplantation have a poor prognosis due to reduced tolerance and suboptimal responses to salvage therapies. Select pts who respond to salvage and achieve prolonged remissions may benefit from second transplantations. We hypothesized that less toxic conditioning, as well as advancements in supportive care and salvage therapies, may improve outcomes when pts relapse after transplantation. Among 72 pts with high risk and refractory leukemias consecutively enrolled to receive a RIST from 2002–05, we describe outcomes for the 31 pts who relapsed. The preparative regimen consisted of fludarabine 30 mg/m2/d IV (D-7 to D-3), Campath-1H 20 mg/d IV (D-7 to D-3), melphalan 140 mg/mg2 IV (D-2) and tacrolimus for post-transplantation immunosuppression. Of the 31 pts who relapsed after transplantation, 23 had AML/MDS, 3 had CML, 2 had ALL, 2 had leukemic phase of mantle cell lymphoma and 1 had mast cell leukemia (MCL). Only 4 pts had achieved a complete remission (CR) at initial transplantation. 16 pts (52%) had HLA-identical sibling donors, 1 (3%) had a mismatched related donor and 15 (47%) had unrelated donors. The median age was 51 years (range 20–68), and the median time from initial transplantation to relapse was 4 months (range 1–14). After relapse the median follow-up for survivors was 6.6 months (range 2–28) and the median overall survival (OS) was 7.8 months (95% CI, 4.2–13.5) (Figure 1). The median whole blood or marrow donor chimerism at relapse was 71% (range 0–99%). The median marrow blast percentage at relapse was 21% (range 0–99%); 8 pts had <5% blasts at relapse (AML/MDS=3, CML=3, MCL=1, ALL=1). 3 pts who received no therapy died of progression. 28 pts (90%) received salvage therapy with chemotherapy or biological agents (n=10), DLI (n=4) or a second allogeneic transplantation with or without reinduction (n=14). Among those treated, 15/28 (54%) died, 4 from treatment related mortality (TRM) and 11 from disease. 16/28 (57%) achieved a CR, and 11 remain in remission. In a univariate analysis, relapse >100 days after transplantation (n=9, P=.02) and marrow blast count <5% at relapse (n=10, P=.005) were associated with increased OS. Younger age (p=.12) and higher donor chimerism (p=.90) at relapse were not associated with OS. For the 14 pts who received a second transplantation, the median survival was 6 months; 5 remain alive and 4 are in remission with a median follow-up of 5.7 months. In summary, modern salvage therapy, including second transplantation, is relatively well tolerated in pts who relapse after RIST, perhaps secondary to the reduced toxicity of the initial conditioning regimen or improvements in salvage and supportive care. However, although these therapies prolong responses and improve OS, disease progression remains problematic. Longer remission duration and low burden of disease at relapse are favorable prognostic features for pts who relapse after RIST. Interestingly, residual donor chimerism at relapse is relatively high, an observation which could be exploited when designing alternative treatment strategies.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal