Abstract
Conditioning regimens using in vivo alemtuzumab (Campath-1H, humanized anti-CD52) are characterized by low rates of acute and chronic GVHD, but may also result in delayed immune reconstitution. Optimization of such regimens will depend on an understanding of the relation between alemtuzumab exposure, immune reconstitution and GVHD. We have conducted a prospective study of fludarabine 30 mg/m2/d x 5 days, melphalan 140 mg/m2 x 1 day and alemtuzumab 20 mg/d x 5 days as conditioning for related and unrelated allografts. Using an enzyme-linked immunosorbent assay (ELISA), we determined serum free and total Campath levels in 46 patients with hematologic malignancies (45) or sickle cell disease (1) on day 0, day 7, day 14, day 28, day 50, day 75, day 100, day 150 and at one year after transplant (HSCT). 26 (57%) had a matched sibling donor, 16 (35%) a matched unrelated donor (MUD) and 4 (9%) a mismatched related or unrelated donor. 44 pts engrafted and are included in the analysis.
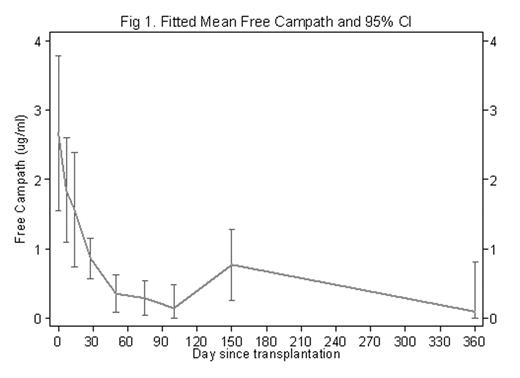
Median follow up for survivors was 2.8 years. Grade II–IV aGVHD occurred in 8 pts after a median of 42 days (range 22 to 60). Eight pts developed cGVHD after a median of 107 days (range 89–140). 15/41 (37%) at risk pts developed CMV reactivation. The half-life of free alemtuzumab (fA) was 26 days after HSCT with wide interpatient variation in fA pharmacokinetics (e.g. Coefficient of variation was 138% on day 0). On day 0, 1 patient had an undetectable level of fA. By day 28, 50, and 100, there were 6 (14.6%), 12 (35.3%), and 13 (52%) pts with undetectable fA, respectively. Figure 1 shows the fitted means and 95% confidence intervals of fA over time.
Using log-rank and Cox proportional hazard models, there was no association between fA on day 0, day 28, or the last available fA, and development of acute GVHD. However, pts with higher average free and total Campath levels in the first month had a lower risk of developing cGVHD (p=0.02). The median fA concentration in the first month for pts with cGVHD was 0.32 (inter-quarter range IQR: 0.22–0.41), as compared with 0.97 (IQR: 0.23–3.31) in those without cGVHD.
No significant association between absolute lymphocyte count and fA concentration was found after adjusting for time (p=0.28). Finally, among pts at risk, a higher fA concentration on day 0 (p=0.002), and in the first month (p=0.003) was significantly associated with CMV viremia.
In summary, the estimated half-life of serum fA is 26 days after HSCT, but with considerable interpatient variability. Higher concentrations of fA were associated with a decreased incidence of cGVHD, but an increased risk of CMV reactivation. In contrast to a previous preliminary analysis, no association existed between fA and lymphocyte reconstitution. Variation in alemtuzumab pharmacokinetics may predict important clinical outcomes, such as cGVHD and CMV reactivation. Future studies are warranted to determine an optimal alemtuzumab exposure that hastens immune reconstitution while minimizing chronic GVHD.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal