Abstract
Between 1997 and 2004, 138 patients with hematological malignancies had an HLA-identical sibling peripheral blood stem cell transplant (PBSCT). Preparative regimen was TBI (12–13.6Gy), cyclophosphamide 120mg/kg +/− fludarabine 125mg/m2. T-cell dose was adjusted to 0.2-1 x 105 CD3+ cells/kg. CD34 dose was 2.7 – 15.9 x 106/kg (median 5.9). Patients without ≥ grade 2 acute GVHD received 1 or 2 donor lymphocyte infusions (DLI) of 107 CD3+ cells/kg between days 45 and 100. For GVHD prophylaxis, all patients received cyclosporine (CSA) following the DLI for a minimum of 6 months. In addition 72 patients received CSA in the first 6 weeks post PBSCT and 66 received no CSA immediately post-transplant. Patients were aged between 10–56 (median 34 years). Seventy-seven patients with CML-CP (42), acute leukemia in first remission (22) or MDS RA (10) were designated as standard risk (SR) for transplant outcome. Sixty-one patients with more advance or refractory disease were designated as high risk (HR) for transplant outcome. Seven patients, distributed in both groups had CLL, NHL, MM and CMML. Overall survival, relapse and TRM were 58 ± 4.5%, 40.2 ± 5.5% and 18.4 ± 3.4% respectively after a median follow up of 4 years. Twenty-two patients did not receive DLI, 70 received one and 46 received two DLI. Twenty-three patients had TRM, 2 from graft failure, 5 from acute or chronic GVHD. Fifty two (37%) developed ≥ grade II, and 21 (15%) patients grade III-IV acute GVHD. Forty two (30%) had limited and 30 (22%) extensive chronic GVHD. In univariate Kaplan-Meier analyses standard risk disease, cGVHD, single DLI and day 30 lymphocyte count (LC30) above median, favorably affected overall survival (DLI p=0.002; LC30 p=0.0002, all other variables p<0.0001). Risk status was the strongest factor predicting relapse (28.8 ± 8% and 58.4 ± 7% in SR and HR patients respectively p<0.0001). Fludarabine, degree of T-cell depletion, age, cyclosporine schedule and CD34 dose were not significant.
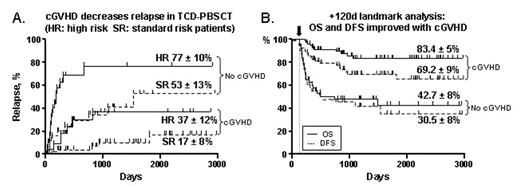
In a Cox regression analysis, only cGVHD (RR, 4.268; p=0.001; 95% CI=1.77–10.25) and standard risk (RR, 0.146; p<0.001; 95%CI=0.06–0.35) remained as independent predictive factors for outcome (Figure A). On landmark analysis after day +120, cGVHD was associated with better OS (p<0.0001) and DFS (p=0.0006) (Figure B), and relapse (21.7± 6% and 51.5 ± 11% in patients with and without cGVHD p= 0.002).
Aggressive T-cell depletion, combined with relatively high doses of CD34+ cells had proven to be a key strategy to minimize TRM and severe aGVHD. Similar to unmanipulated PBSCT this approach appears to provide a protective effect of chronic GVHD, but with low late mortality.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal