Abstract
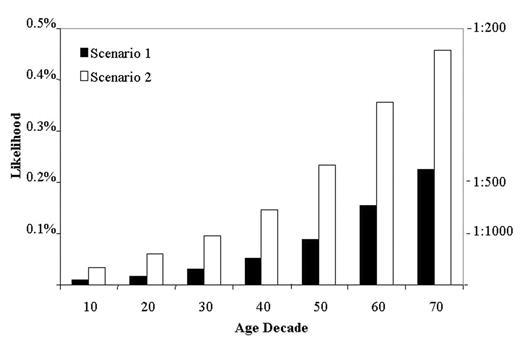
HCT effectively treats a variety of malignant diseases. Availability of suitable grafts limits application in some cases, prompting the establishment of banks to store umbilical cord blood for later personal or family use. The likelihood of utilizing stored cells depends, in part, on the likelihood of developing a condition for which HCT is indicated. This study estimates the latter likelihood based on data for current HCT use as reported to the CIBMTR from 2001 through 2003. First, age-related incidences of HCT were calculated; then, using the cumulative incidence function, we calculated the lifetime likelihood under two scenarios. In scenario 1, we calculated the likelihood of receiving an autologous HCT by age, in decades, from birth to 70 years. In scenario 2, we calculated the likelihood of being a candidate for either an autologous or an allogeneic HCT. This likelihood was derived from the number of HLA-identical sibling HCTs multiplied by three (to account for patients considered acceptable candidates but lacking an HLA-matched sibling donor) in addition to the number of autologous HCT. The number of HCT performed represented fewer than 20% of the malignant diagnoses most commonly treated with HCT, according to Surveillance, Epidemiology and End Results (SEER) data. After the second decade of life, the age-related incidences of HCT under both scenarios steadily increased with age. The cumulative incidences for scenario 1 ranged from 0.02% (at age 20) to 0.23% (at age 70); for scenario 2 they ranged from 0.06% (at age 20) to 0.46% (at age 70) (Figure). Given the current indications for HCT, the lifetime likelihood of undergoing an autologous HCT or being a candidate for HCT is about 1 in 400 and 1 in 200, respectively. How closely these estimates correspond to the likelihood that a stored cord blood unit is used depends upon several conditions including a) sufficient number of stem cells; b) satisfactory stem cell quality after the storage period; and, c) relative attractiveness, in particular clinical situations, of cord blood cells compared to other graft sources (e.g. peripheral blood or bone marrow).
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal