Abstract
Chemokines play a pivotal role in homeostatic and inflammatory migration of naive and activated natural killer (NK) subsets. Recent studies have shown that aberrant chemokine receptor expression on certain immune cells underlies the pathogenesis of clinical conditions in which recruitment of such cells is altered. Progressive accumulation of activated NK cells, subsequently resulting in the formation of chronic granulomatous lesions in the respiratory tract and the skin, has been described in a number of patients with transporter associated with antigen processing 2 (TAP-2) deficiency in the later stages of disease. Therefore, the goal of the present study was to elucidate whether the dysregulation of chemoattracting receptor expression on NK cells could explain abnormal navigation of these cells in TAP-2 deficiency. High-throughput proteomic comparison, followed by verification with flow cytometry, revealed that chronically activated NK cells derived from 3 newly identified patients with TAP-2 deficiency consistently expressed aberrant levels of CC chemokine receptor 2 (CCR2) chemokine receptor in vitro and in vivo. This expression pattern translated into specific responsiveness of chronically activated NK cells derived from patients with TAP-2 deficiency to multiple ligands of CCR2. Moreover, the in vivo elevated levels of interleukin-2 (IL-2) and monocyte chemoattractant protein-1 (MCP-1) detected in serum and bronchoalveolar lavage samples derived from these patients highlight the potential involvement of the CCR2 pathway in aberrant NK-cell retention at chronic inflammatory sites.
Introduction
Transporter associated with antigen processing 2 (TAP-2) deficiency is a rare disorder characterized by systemic multiorgan clinical manifestations developing at various stages of disease, all resulting from significantly lower expression levels of major histocompatibility complex (MHC) class 1.1 Defective TAP-2 expression in these patients prevents the assembly of TAP-1/TAP-2 heterodimers that are crucial for importing peptides into the lumen of the endoplasmic reticulum and proper assembly of stable MHC class 1 on the cell surface. This syndrome has drawn the interest of several researchers who wanted to better understand lymphocyte development and behavior in an environment of low MHC class 1 expression and to correlate their observations with clinical symptoms observed during the course of the disease.
At early stages and throughout their first 3 decades of life, patients with TAP-2 deficiency are reported to experience repeated, yet not lethal, respiratory tract infections (mainly sinusitis and recurrent bronchitis).1-3 Studies have shown that despite the low levels of MHC class 1 molecules, these patients do not have complete deficiency of cytotoxic functions because they maintain an altered, but still effective, cell-mediated cytotoxic immune response, including that of natural killer (NK) cells.2 On the other hand, the fact that patients with TAP-2 deficiency do not experience severe NK-mediated, autoimmunelike symptoms at early stages of the disease has drawn extensive research attention3,4 because autologous cells in these patients should have been killed by natural killers. NK cells are a subset of bone marrow–derived lymphocytes that constitutes approximately 10% of peripheral-blood leukocytes (PBLs) and is characterized by a lack of T-cell–receptor (TCR) expression and expression of CD56 (CD3–CD56+). These cells function as a first-line defense mechanism against tumor-transformed and pathogen-infected cells.5 NK cells express a variety of activating and inhibitory receptors that recognize MHC class 1 molecules; thus, the loss of MHC class 1 expression that often occurs after viral infection results in the loss of inhibitory signals and shifts the balance between these 2 receptor families toward cytotoxicity induction against the target cell through specific NK-activating receptors.6 However, it has recently been shown that activated NK cells derived from a number of patients with TAP-2 deficiency up-regulate the inhibitory NK receptor carcinoembryonic antigen–related cell-adhesion molecule 1 (CEACAM1) and partially down-regulate some activating receptors, including NKp46 and natural killer group 2D (NKG2D).3,4 This manipulation of receptor expression facilitates at least partial inhibition of lysis of low-expressing MHC class 1 autologous cells by NK cells while maintaining low, yet effective, expression of activating receptors and ability to combat pathogens.
In spite of these adaptive modifications in immune effector behavior to avoid profound NK-mediated autoimmunity at early stages of life, adult patients with TAP-2 deficiency toward the end of the third decade of life gradually develop multiple chronic necrotizing granulomatous lesions in the skin and the respiratory tract that eventually progress and become lethal.7 Pathologic examination of these lesions reveals that they result from progressive accumulation of activated NK cells (eg, expressed CD69 and MHC class 2 activation markers7 ). The presence of multiple chronic infections was extensively ruled out as a cause for these NK granulomas, thus leaving the question of why activated NK cells are aberrantly recruited and retained in these lesions unanswered.7 Dysregulation of chemokine or chemokine receptor expression could result in pathologic cellular trafficking and behavior in vivo.8 Recently, the aberrant expression of CC chemokine receptor 6 (CCR6) has been shown to underlie the formation of Langerhans-cell granulomatous lesions in histiocytosis X.9 After these observations, we aimed to study whether the granulomatous NK lesions found at late stages in patients with TAP-2 deficiency might be involved in the aberrant trafficking capabilities of chronically activated NK cells from these patients.
We have previously described an Arab-Israeli family with 3 children in whom TAP-2 deficiency was diagnosed.4,10,11 High-throughput proteomic analysis followed by flow cytometry verification revealed that chronically activated NK (CANK) cells derived from patients with TAP-2 deficiency expressed unusually high levels of CCR2 chemokine receptor in vitro and in vivo and subsequently resulted in specific enhanced migration to several CCR2 ligands. Moreover, these patients had constantly elevated serum levels of monocyte chemoattractant protein-1 (MCP-1), a major ligand for CCR2, and significant levels of interleukin-2 (IL-2) and MCP-1 in bronchoalveolar lavage (BAL) samples, thus demonstrating that the conditions required for CCR2 expression and CCR2-mediated NK-cell responsiveness are provided in vivo. Potential implications of our findings on fundamental immunologic scenarios in patients with TAP-2 deficiency are discussed.
Materials and methods
Cell isolation
Blood samples were obtained from previously described patients A, B, and C4,10 with TAP-2 deficiency or from their mother and multiple additional donors and were loaded on Ficoll-density gradient to purify the lymphocyte population. An institutional review board approved these studies, and informed consent was obtained in accordance with the Declaration of Helsinki. Freshly isolated peripheral-blood–derived unactivated NK cells were purified using the human NK cell isolation kit II and the auto-MACS instrument (Miltenyi Biotec, Bergisch-Gladbach, Germany). Bulk polyclonal CANK cultures were grown as previously described.12 Briefly, purified NK cells from peripheral blood were plated at 1 cell/well in 96 U-well plates in RPMI medium supplemented with 10% human serum, 50 U/mL recombinant human IL-2 (Boehringer Mannheim, Indianapolis, IN), and 1 ng/mL phytohemagglutinin (PHA) for 2 weeks. Irradiated feeder cells (2.5 × 104 allogeneic peripheral-blood mononuclear cells (PBMCs) from 2 donors and 5 × 103 RPMI 8866 cell line in each well) were added. Proliferating clones were verified to be positive for CD56 and negative for CD3 markers and were subsequently combined and grown for an additional week to generate bulk polyclonal CANK cell lines. Purity of CANK cell lines was routinely verified to be greater than 99%. Additionally, short-term activation of freshly isolated PBL-derived NK cells was performed in RPMI medium supplemented with 10% human serum and 50 U/mL recombinant human IL-2 for 24, 48, and 72 hours. Chronically activated T-cell lines were generated and cultured similarly after purification of CD3+ T cells with the human T-cell isolation kit II (Miltenyi Biotec). BAL fluid obtained from the different donors was immediately processed and centrifuged. The supernatant was removed and stored in individual aliquots at –70°C, and the cellular fraction was further processed and used to purify NK cells using the human NK cell isolation kit II (Miltenyi Biotec).
CANK cell-membrane preparation and tandem mass spectrometry (MS/MS) analysis of tryptic peptides
Semiquantitative reverse transcription–polymerase chain reaction analysis
Total RNA was isolated from CANK cell lines derived from healthy donors, patients with TAP-2 deficiency, and their mother using the RNeasy Mini Kit (Qiagen, Valencia, CA). cDNA was prepared according to standard protocol. Sequences of CCR2 and actin primers used were previously described.14
Antibodies and quadruple staining
The following fluorochrome-conjugated monoclonal antibodies (mAbs) were used: fluorescein isothiocyanate (FITC)–conjugated anti–human CD56 (Southern Biotechnology Associates, Birmingham, AL) and CyChrome-conjugated anti–human CD3 (BD PharMingen, San Diego, CA). Biotinylated anti–CD16 mAb (Serotec, Oxford, United Kingdom) was used, after which streptavidin-Cy5 (Jackson Immunoresearch, West Grove, PA) was used as a second reagent. As the fourth color, one of the following phycoerythrin (PE)–conjugated antihuman mAbs obtained from R&D Systems (Minneapolis, MN) was used: anti–C-X-C–motif chemokine receptor 1 (CXCR1), anti-CXCR2, anti-CXCR3, anti-CXCR4, anti-CCR1, anti-CCR2, anti-CCR3, anti-CCR4, anti-CCR5, anti-CCR6, or anti-CCR7. When quadruple staining was performed with FITC-conjugated anti–human CX3CR1 mAb (Medical & Biological Laboratories, Nagoya, Japan), the PE-conjugated anti–human CD56 (BD PharMingen) was used.
ELISA
Chemokine concentration in the various samples was determined by performing enzyme-linked immunosorbent assay (ELISA) with the equivalent quantikine kit (R&D Systems).
In vitro cell-migration assay
NK cells (2 × 105; 100 μL) were loaded into each Transwell filter (5-μm pore filter; 24-well cells clusters; Corning, Corning, NY). Filters were then plated in each well containing 600 μL medium supplemented with various chemokines (obtained from R&D Systems), as indicated in each figure. At least 4 wells were used for each chemokine concentration. To determine nonspecific or background migration, 6 wells that did not contain any chemokine were used as controls. After 3 hours of incubation at 37°C, 5% CO2, the upper chambers were removed and cells in the bottom chamber were collected, counted, and analyzed by flow cytometry. Migration index was calculated by dividing the number of cells migrating in the presence of chemokines by those migrating toward medium only (control).
Results
High-throughput proteomic analysis of chronically activated NK-membrane–enriched fractions
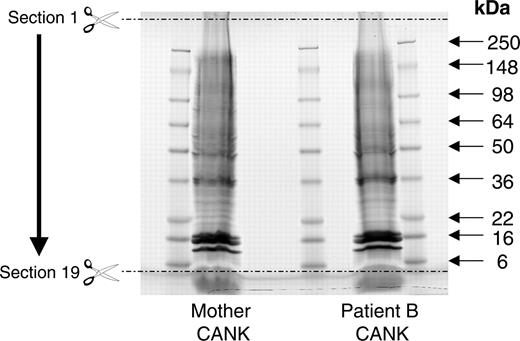
Sustained activation of NK cells in inflammatory sites has been documented in patients with TAP-2 deficiency and has been attributed to recurrent infections and chronic inflammation.3 Furthermore, it has been suggested that chronic activation might lead to the disruption of self-tolerance by NK cells at later stages of the disease.3 Therefore, we chose a classic in vitro activation model for the generation of bulk polyclonal NK cultures3,12 to study the phenotypes of CANK cells in patients with TAP-2 deficiency and in healthy donors. This approach overcame our limited ability to obtain sufficient amounts of blood samples and isolated NK cells from pediatric patients with TAP-2 deficiency. To study how the migratory capability of CANK cells derived from patients with TAP-2 deficiency might be altered, we applied experiments involving a high-throughput MS/MS proteomics-based comparison between CANK-membrane–enriched fractions from TAP-2–deficient patient B and his healthy mother. After preparing membrane-enriched fractions from purified CANK cultures of these 2 donors, the complex membrane protein mixtures were separated into 19 molecular mass fractions by 1-dimensional gel electrophoresis followed by excision of equally spaced bands (Figure 1). The spectra were searched against a human database using a probability-based scoring algorithm. This query resulted in a list of more than 1000 proteins identified from CANK cells in both samples (Supplemental Tables S1 and S2, respectively [available at the Blood website by clicking the Supplemental Tables link at the top of the online article]). Preliminary analysis confirmed known differences between CANK cells derived from healthy donors and from patients with TAP-2 deficiency. For example, MHC class 1–associated protein-derived peptides were barely detectable in patient B's sample when compared with his mother's sample (Table 1). In addition, CEACAM1-derived peptides were specifically detected in patient B's sample (Table 1), confirming the previously reported abundant up-regulation of this receptor in patients with TAP-2 deficiency.4,10
Identified MHC class 1 and trafficking-regulating receptors after MS/MS proteomic analysis of mother and patient B CANK-cell–derived, membrane-enriched protein fractions
Protein family and description . | Accession no. . | Section no. . | Protein-derived peptides, total score . |
|---|---|---|---|
| Mother | |||
| MHC class 1-related proteins | |||
| MHC class 1 antigen | Q9TQG6 | 11 | 65.38 |
| MHC class 1 antigen | Q9GJF5 | 12 | 107.24 |
| MHC class 1 antigen | Q95HA7 | 17 | 48.14 |
| HLA-C heavy chain | Q30203 | 10 | 27.24 |
| HLA-A10 α-chain | HLHU10 | 11 | 183.65 |
| HLA-A2-α-2 | I56009 | 18 | 22.04 |
| HLA-A cell-surface antigen | I54412 | 12 | 97.23 |
| HLA-CW fragment | Q29645 | 11 | 44.98 |
| β2-microglobulin | AAB25312 | 19 | 73.19 |
| MHC class 1 independent inhibitory receptors | |||
| CEACAM1 (CD66a) | ND | ND | ND |
| Trafficking-regulating molecules | |||
| ICAM-3 | S28904 | 4 | 65.76 |
| LFA-1 | ITAL_HUMAN | 3 | 518.12 |
| GPR48 | Q9NYD1 | 3 | 25.76 |
| CD44 | Q9NRY3 | 18 | 39.02 |
| CXCR3 | Q9P2T5 | 16 | 156.12 |
| CCR2 | ND | ND | ND |
| Patient B | |||
| MHC class 1—related proteins | |||
| HLA-C heavy chain | Q30204 | 11 | 30.4 |
| MHC class 1 antigen | Q9GJ38 | 10 | 40.62 |
| MHC class 1 independent inhibitory receptors | |||
| CEACAM1 (CD66a) | P13688 | 19 | 187.23 |
| Trafficking-regulating molecules | |||
| ICAM-3 | S28904 | 4 | 59.08 |
| LFA-1 | ITAL_HUMAN | 3 | 400.79 |
| GPR48 | Q9NYD1 | 3 | 32.67 |
| CD44 | Q9NRY3 | 18 | 27.98 |
| CXCR3 | Q9P2T5 | 16 | 139.66 |
| CCR2 | P41597 | 7 | 341.29 |
Protein family and description . | Accession no. . | Section no. . | Protein-derived peptides, total score . |
|---|---|---|---|
| Mother | |||
| MHC class 1-related proteins | |||
| MHC class 1 antigen | Q9TQG6 | 11 | 65.38 |
| MHC class 1 antigen | Q9GJF5 | 12 | 107.24 |
| MHC class 1 antigen | Q95HA7 | 17 | 48.14 |
| HLA-C heavy chain | Q30203 | 10 | 27.24 |
| HLA-A10 α-chain | HLHU10 | 11 | 183.65 |
| HLA-A2-α-2 | I56009 | 18 | 22.04 |
| HLA-A cell-surface antigen | I54412 | 12 | 97.23 |
| HLA-CW fragment | Q29645 | 11 | 44.98 |
| β2-microglobulin | AAB25312 | 19 | 73.19 |
| MHC class 1 independent inhibitory receptors | |||
| CEACAM1 (CD66a) | ND | ND | ND |
| Trafficking-regulating molecules | |||
| ICAM-3 | S28904 | 4 | 65.76 |
| LFA-1 | ITAL_HUMAN | 3 | 518.12 |
| GPR48 | Q9NYD1 | 3 | 25.76 |
| CD44 | Q9NRY3 | 18 | 39.02 |
| CXCR3 | Q9P2T5 | 16 | 156.12 |
| CCR2 | ND | ND | ND |
| Patient B | |||
| MHC class 1—related proteins | |||
| HLA-C heavy chain | Q30204 | 11 | 30.4 |
| MHC class 1 antigen | Q9GJ38 | 10 | 40.62 |
| MHC class 1 independent inhibitory receptors | |||
| CEACAM1 (CD66a) | P13688 | 19 | 187.23 |
| Trafficking-regulating molecules | |||
| ICAM-3 | S28904 | 4 | 59.08 |
| LFA-1 | ITAL_HUMAN | 3 | 400.79 |
| GPR48 | Q9NYD1 | 3 | 32.67 |
| CD44 | Q9NRY3 | 18 | 27.98 |
| CXCR3 | Q9P2T5 | 16 | 139.66 |
| CCR2 | P41597 | 7 | 341.29 |
ND indicates not detected.
When we examined potential differences in the detection of peptides derived from molecules involved in the regulation of CANK-cell migration, specific peptides derived from CCR2 chemokine receptor were detected in patient B's sample, providing a total score of 341.29, whereas no such peptides were detected from his mother sample (Table 1). Peptide levels such as those of CXCR3, CD44, and lymphocyte function–associated antigen 1 (LFA-1), derived from other molecules involved in NK-cell migration, were similarly detected in both samples (Table 1). Taken together, this general screening provided us with a “lead” suggesting a significant up-regulation of CCR2 receptor in CANK cells of patients with TAP-2 deficiency that required further evaluation.
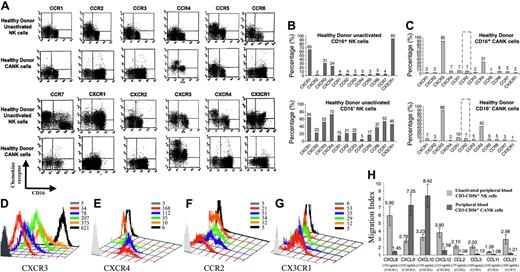
Characterization of chemokine receptor expression on human NK subsets on chronic activation
Human NK cells can be divided based on their cell-surface levels of CD56 (NCAM1) and CD16 (FcγRIII) into 2 distinct subsets—CD56dimCD16+ NK cells, which constitute approximately 90% of circulating peripheral-blood NK cells, and CD56brightCD16low NK cells, which constitute most of the remaining cells.15 The CD56dim subset is more cytotoxic, whereas the CD56bright subset is more potent at cytokine secretion and is found in the T-cell paracortical area in human lymph nodes.16,17 Previous works that characterized chemokine receptor expression on resting (unstimulated) NK subsets have demonstrated a dramatic difference in chemokine receptor expression between them.14,18 Our analysis of polyclonal unactivated (freshly isolated) purified NK cells obtained from 23 healthy donors verified the previously reported obvious differences in chemokine receptor expression patterns between unactivated CD56dim and CD56bright NK subsets (Figure 2A-B).14,18 Before examining NK chemokine receptor expression on CANK cells in patients with TAP-2 deficiency, we wanted to thoroughly characterize normal levels for chemokine receptor expression on healthy donor–derived CANK cells generated in our in vitro activation model system and with our reagents to define normal baseline expression levels for each receptor on CANK cells. Additionally, we wanted to examine whether there are different patterns of chemokine receptor expression on CD56dimCD16+ and CD56brightCD16low NK subsets after prolonged activation.
One-dimensional gel separation of CANK cell membrane–enriched fractions. One hundred micrograms of CANK cell membrane–enriched fractions obtained from patient B and his mother were separated on 4% to 20% Tris-glycine gel. Nineteen equally spaced sections between 250 kDa and 6 kDa were excised from each fraction and were subsequently used for proteomic analysis.
One-dimensional gel separation of CANK cell membrane–enriched fractions. One hundred micrograms of CANK cell membrane–enriched fractions obtained from patient B and his mother were separated on 4% to 20% Tris-glycine gel. Nineteen equally spaced sections between 250 kDa and 6 kDa were excised from each fraction and were subsequently used for proteomic analysis.
Our results show that sustained NK stimulation induced profound changes in chemokine receptor cell-surface profiles. In all polyclonal CANK-cell cultures derived from 23 healthy donors, this form of activation resulted in significant down-regulation of all chemokine receptors examined on NK cells on each subset before activation, except for CCR4 and, more prominently, CXCR3, which were constantly up-regulated after chronic activation (Figure 2A-C). These results correlate with the results of proteomic analysis performed on the CANK sample of the patient's mother because CXCR3 receptor–derived peptides were detected at significant levels from both CANK samples (Table 1), but the relatively lower number of cells and the lower-intensity level of expression of other chemokine receptors (including that of CCR4) observed by flow cytometry (Figure 2B-D) were not high enough to meet the detection threshold set in the proteomic analysis. No significant differences were observed in chemokine receptor expression between chronically activated CD56dimCD16+ and CD56bright CD16low NK subsets (Figure 2C). Importantly, our results confirm findings in several recently published papers describing alterations in chemokine receptor expression on chronically activated NK cells generated by a similar stimulation protocol. Sentman et al19 show that human uterine NK clones prepared under the same culture conditions used in our study up-regulated CXCR3 and down-regulated CXCR1, CXCR2, CXCR4, and CCR7 receptors. Some clones in the same article expressed low levels of CCR5 receptor. Similarly, we observed that a certain subset of CD16– NK cells, known to populate the maternal uterine mucosa, specifically retained positive expression of CCR5 receptor (Figure 2A). Moreover, the same authors show that PBL-derived CD56bright and CD56dim subsets up-regulate CXCR3 receptor on their cell surfaces on stimulation with IL-2 only. Beider et al20 showed that lymphokine-activated human NK cells up-regulated CXCR3 receptor and down-regulated CCR5, CXCR1, and CXCR4 molecules—processes known to be dependent on these receptors—resulting in decreased in vivo recruitment and retention in the bone marrow and spleens of NOD/SCID mice. Several additional papers that induced NK activation through stimulation with IL-2 alone also supported our data. CCR7 receptor has been shown to be down-regulated on NK cells after IL-2 activation,21,22 whereas the CCR4 molecule has been shown to be induced on activated NK cells.22-24 CXCR4 has been shown to be down-regulated through stimulation with different cytokines, including IL-2 (Figure 2E) and IL-15, whereas TGF-β has been proven as a potent inducer of CXCR4 on NK subsets.14,22
Nonetheless, the chemokine receptor profile on CANK cells characterized here might seem to contradict findings in certain papers that described the expression of some of these receptors on activated NK cells. However, methodologic differences in the generation of activated NK cells can explain the differences between these results. Previous studies have shown that activated NK cells incubated with IL-2, irradiated target cells, or both for up to 10 days up-regulated CCR2 expression and demonstrated enhanced responsiveness to CCR2 ligands.25-27 However, unlike the CANK cells prepared in this study, the activation method used in these papers did not include adding PHA or growing the cells on mixed irradiated lymphocytes from different donors as feeder cells (in other words, the cells were not stimulated with cytokines secreted from the mixed lymphocyte reaction). Thus, such differences in activation methods might result in a different chemokine receptor repertoire on the stimulated NK cells. Indeed, when we stimulated polyclonal unactivated NK cells with IL-2 only, we observed an up-regulation in the CCR2 receptor at 24 hours, and the receptor was still detectable at the NK-cell surface 72 hours after stimulation (Figure 2F). Such surface expression levels on IL-2–activated NK cells correlates with the previously enhanced responsiveness of these cells to CCR2 receptor ligands,25-27 whereas undetectable levels of CCR2 receptor on CANK cells support their lack of responsiveness to CCR2 ligands (Figure 2H). Moreover, the staining pattern presented in Figure 2F rules out the possibility that we obtained false-negative staining for CCR2 on CANK cells because this reagent proved to have positive reactivity against unstimulated and IL-2–stimulated NK cells (Figure 2F). Similarly, the expression of CCR5 receptor on activated NK cells observed by Nieto et al,25 but not on CANK cells in our study (Figure 2A, C), can be attributed to the same differences in NK culturing conditions already explained. Notably, the fact that CD16– unactivated NK cells, but not CANK cells, expressed high levels of CCR5 receptor (Figure 2A) rules out the possibility that our observed CCR5 phenotype on CANK cells was caused by reagent limitation. Regarding the CX3CR1 receptor, we observed that unactivated and IL-2–stimulated NK cells, but not CANK cells, had significant expression levels of this receptor (Figure 2G). Indeed, Fraticelli et al28 demonstrated that IL-2–activated NK cells transcribed the CX3CR1 receptor and that further activation of these cells by cross-linking the CD16-activating receptor resulted in a pronounced down-regulation of this receptor. Thus, the fact that CANK cells used in this study were cultured with RPMI 8866 target cells that express ligands for several NK-activating receptors could explain the undetectable surface expression of CX3CR1 on CANK cells. Finally, Inngjerdingen et al22 used a different activation method for NK cells that relied on IL-2 stimulation and on separating NK cells into adherent and nonadherent subsets. Despite the methodologic differences, they observed a similar expression pattern for CXCR3, CXCR4, CCR4, and CCR7 receptors when NK cells were activated with IL-2. CXCR1, CXCR2, CCR5, and CX3CR1 receptors were not detected on unactivated or activated NK cells in the same study. However, the fact that several published studies14,18,20,21,28-30 were able to characterize functional expression of these receptors on unactivated CD16+ or CD16– NK subsets supports the possibility that reagent limitations were responsible for the inability to detect these receptors in the earlier works.
Chemokine receptor distribution on the cell surfaces of healthy donor–derived NK-cell subsets. Unactivated peripheral NK cells and CANK cell lines were generated and quadruple stained, as described in “Materials and methods.” (A) Chemokine receptor expression on healthy donor CD16+ and CD16– unactivated NK and CANK cells. (B-C) Representative chemokine receptor expression values on unactivated NK and CANK cells based on their CD16 phenotype. Indicated values represent the percentage of cells of the total cell population positive for a certain chemokine receptor. (D-G) Time-dependent changes in chemokine receptor expression on NK cells stimulated with 50 U/mL IL-2 in comparison with CANK cells. (D) CXCR3 changes on CD16+ NK. (E) CXCR4 changes on CD16– NK. (F) CCR2 changes on polyclonal NK. (G) CX3CR1 changes on CD16+ NK. Values indicate mean fluorescence intensity (MFI) values for each staining. (H) Migration assay for healthy donor polyclonal unactivated NK (light gray) and CANK cell lines (dark gray) to multiple chemokines at optimal concentration levels was performed, as described in “Materials and methods.” Matching receptor and concentration used for each chemokine are indicated in brackets. Results are from 1 representative experiment of 3 to 23 experiments performed.
Chemokine receptor distribution on the cell surfaces of healthy donor–derived NK-cell subsets. Unactivated peripheral NK cells and CANK cell lines were generated and quadruple stained, as described in “Materials and methods.” (A) Chemokine receptor expression on healthy donor CD16+ and CD16– unactivated NK and CANK cells. (B-C) Representative chemokine receptor expression values on unactivated NK and CANK cells based on their CD16 phenotype. Indicated values represent the percentage of cells of the total cell population positive for a certain chemokine receptor. (D-G) Time-dependent changes in chemokine receptor expression on NK cells stimulated with 50 U/mL IL-2 in comparison with CANK cells. (D) CXCR3 changes on CD16+ NK. (E) CXCR4 changes on CD16– NK. (F) CCR2 changes on polyclonal NK. (G) CX3CR1 changes on CD16+ NK. Values indicate mean fluorescence intensity (MFI) values for each staining. (H) Migration assay for healthy donor polyclonal unactivated NK (light gray) and CANK cell lines (dark gray) to multiple chemokines at optimal concentration levels was performed, as described in “Materials and methods.” Matching receptor and concentration used for each chemokine are indicated in brackets. Results are from 1 representative experiment of 3 to 23 experiments performed.
The changes in chemokine receptor expression on NK cells (Figure 2A-C) were in exact correlation with the migration ability of polyclonal unactivated and CANK cells. The latter migrated more efficiently only to CXCR3 ligands (CXCL9 and CXCL10), whereas ligands for CXCR1, CXCR4, CCR2, CCR3, CCR5, and CCR7 were more potent in inducing the migration of unactivated peripheral NK cells (Figure 2H).
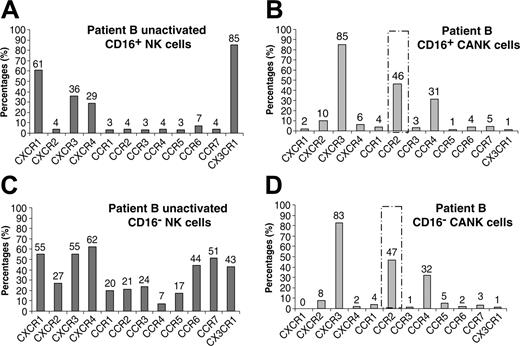
Unusually high expression levels of CCR2 chemokine receptor on CANK cells in patients with TAP-2 deficiency
We next wanted to verify whether the significant detection of CCR2-derived peptides from the CANK cells of TAP-2–deficient patient B (Table 1) was a result of an alteration in CCR2 receptor expression. Remarkably, surface expression characterization of chemokine receptors in patient B CANK cells showed a profound overexpression of CCR2 receptor in CD16+ and CD16– NK subsets (Figure 3B, D) compared with healthy donor–derived CANK cells (Figure 2C). No differences were observed in other chemokine receptors between healthy donor–derived and patient B CANK cells (Figures 2A, C, 3A, C). Additionally, freshly isolated CD16+ and CD16– unactivated NK cells from patient B expressed a chemokine receptor profile similar to that of healthy donors (Figures 2, 3), suggesting that the aberrant expression of CCR2 receptor in patient B NK cells was observed only after chronic activation.
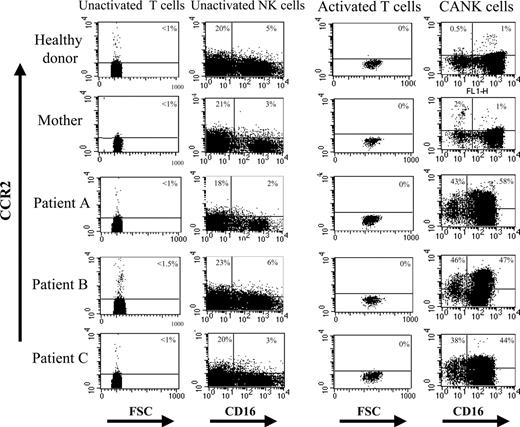
When analyzing CCR2 expression on NK cells from other family members with TAP-2 deficiency, we found similarly up-regulated CCR2 receptor on the CANK cells of patients A and C but not on freshly isolated, unactivated NK cells (Figure 4). None of the 23 CANK cell lines generated from healthy donors (age range, 8-30 years) or from the patients' mother displayed more than 2% CCR2-positive NK cells (Figure 4). This pattern of CCR2 expression on CANK cells was consistent in patients with TAP-2 deficiency because CANK lines generated from 2 additional samples obtained 2 and 5 months later from patients A, B, and C displayed similar up-regulation of the CCR2 receptor (data not shown). Unactivated and chronically activated T-cell lines generated from patients A, B, and C did not express significant levels of CCR2 receptor (Figure 4), suggesting that the prominent expression of this receptor on the patients' CANK cells was not caused by a generalized nonspecific effect of activation on various TAP-2–deficient lymphocyte subsets but, rather, was restricted to NK cells. One possibility to account for the aberrant expression of CCR2 on TAP-2–deficient CANK cells was that these patients experienced several episodes of respiratory tract infections, which might have caused alterations in NK-cell behavior. However, the fact that the CANK cell lines used in our studies were cultured for more than 2 weeks in vitro before analysis makes this notion unlikely. Furthermore, unactivated NK cells and CANK cell lines purified from blood samples obtained from 6 patients (age range, 4-17 years) with ongoing respiratory tract infections of different causes showed no up-regulation in the expression of CCR2 receptor (data not shown).
Chemokine receptor distribution on the NK-cell surface of patient B. Unactivated peripheral NK cells and CANK cell lines were generated and quadruple stained, as described in “Materials and methods.” Chemokine receptor expression on TAP2-deficient patient B CD16+ unactivated (A) and CANK (B) cells and on patient B–derived CD16– (C) unactivated and CANK (D) cells. Indicated values represent the percentage of the total cell population of cells positive for a certain chemokine receptor. Results are from 1 representative experiment of 3 experiments performed.
Chemokine receptor distribution on the NK-cell surface of patient B. Unactivated peripheral NK cells and CANK cell lines were generated and quadruple stained, as described in “Materials and methods.” Chemokine receptor expression on TAP2-deficient patient B CD16+ unactivated (A) and CANK (B) cells and on patient B–derived CD16– (C) unactivated and CANK (D) cells. Indicated values represent the percentage of the total cell population of cells positive for a certain chemokine receptor. Results are from 1 representative experiment of 3 experiments performed.
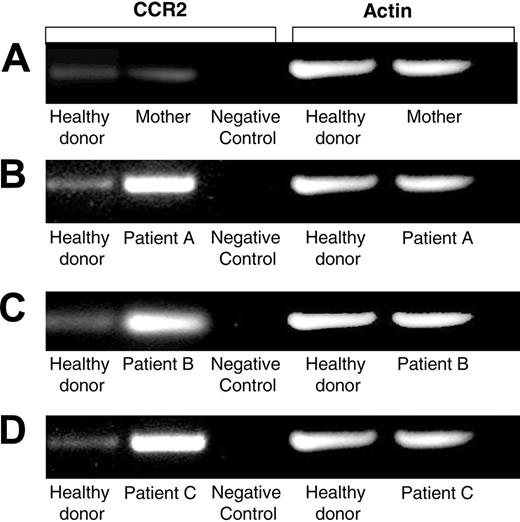
CCR2 mRNA level is elevated in the CANK cells of patients with TAP-2 deficiency
To determine whether the up-regulation of cell-surface–expressed CCR2 on CANK lines from patients with TAP-2 deficiency was a result of higher transcription levels of this gene, we performed semiquantitative reverse transcription–polymerase chain reaction (RT-PCR) comparison analysis between pooled cDNA obtained from 7 healthy donor–derived CANK cells lines and cDNA samples obtained from family members with TAP-2 deficiency. Indeed, this analysis clearly demonstrated that CCR2 transcripts were significantly more abundant in the CANK cells of patients A, B, and C than in those of the healthy donors (Figure 5), whereas the CANK cell line of the healthy mother displayed levels of CCR2 transcripts comparable to those of the healthy donors. These results show that elevated transcription levels of the CCR2 gene contribute to the up-regulation of cell-surface expression CCR2 receptor on CANK cells derived from the TAP-2–deficient patients. However, because chemokine receptors are known to be sensitive to a variety of posttranslational modifications,14,31 these results do not rule out the possibility that such processes might also assist in the up-regulation of the observed CCR2 chemokine receptor at the protein level.
Specific augmented expression of CCR2 on CANK cells derived from patients with TAP-2 deficiency. Surface expression levels of CCR2 on unactivated, CANK, and activated T cells derived from multiple blood samples obtained from healthy donors (representative staining for 1 of 23 healthy donors), the mother of patients A, B, and C with TAP-2 deficiency, and the patients themselves. Indicated values represent the percentages of cells positive for CCR2 of that total lymphocyte subset. Results are from 1 representative experiment of 3 experiments performed on lymphocytes and cell lines generated on 3 independent occasions from each donor.
Specific augmented expression of CCR2 on CANK cells derived from patients with TAP-2 deficiency. Surface expression levels of CCR2 on unactivated, CANK, and activated T cells derived from multiple blood samples obtained from healthy donors (representative staining for 1 of 23 healthy donors), the mother of patients A, B, and C with TAP-2 deficiency, and the patients themselves. Indicated values represent the percentages of cells positive for CCR2 of that total lymphocyte subset. Results are from 1 representative experiment of 3 experiments performed on lymphocytes and cell lines generated on 3 independent occasions from each donor.
Increased mRNA levels of CCR2 receptor in TAP-2–deficient CANK cells. Semiquantative RT-PCR analysis for CCR2 mRNA levels was performed on various cDNA libraries obtained. Healthy donor–derived cDNA was prepared from an mRNA pool purified from equal numbers of CANK cells from 7 healthy persons. cDNA obtained from 1106 melanoma cell line was used as a negative control for CCR2 receptor. RT-PCR analysis was performed to compare intensities of CCR2 levels on CANK cell lines between healthy donors and (A) the mother of patients A, B, and C with TAP-2 deficiency, (B) patient A, (C) patient B, and (D) patient C. Results are from 1 independent experiment of 4 experiments performed.
Increased mRNA levels of CCR2 receptor in TAP-2–deficient CANK cells. Semiquantative RT-PCR analysis for CCR2 mRNA levels was performed on various cDNA libraries obtained. Healthy donor–derived cDNA was prepared from an mRNA pool purified from equal numbers of CANK cells from 7 healthy persons. cDNA obtained from 1106 melanoma cell line was used as a negative control for CCR2 receptor. RT-PCR analysis was performed to compare intensities of CCR2 levels on CANK cell lines between healthy donors and (A) the mother of patients A, B, and C with TAP-2 deficiency, (B) patient A, (C) patient B, and (D) patient C. Results are from 1 independent experiment of 4 experiments performed.
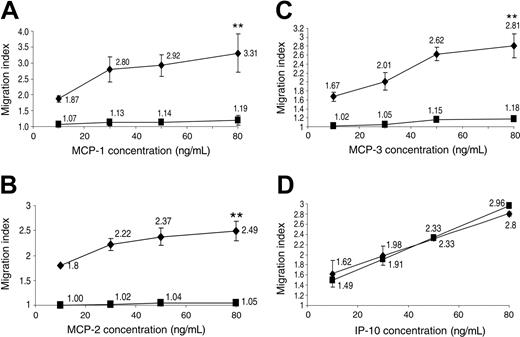
Profound migration of CANK cells from patients with TAP-2 deficiency to CCR2 ligands
The functional importance of CCR2 chemokine receptor expression on the various CANK cell lines generated was evaluated through in vitro transwell migration assay. Remarkably, data presented in Figure 6 show that in each of the 3 separate experiments performed, TAP-2–deficient CANK cell lines displayed prominent and specific migration to different CCR2 ligands: MCP-1, MCP-2, and MCP-3 (Figure 6A-C). In contrast, CANK cells derived from several healthy donors and the patients' mother, in correlation with the low CCR2 receptor expression revealed by flow cytometry (Figures 2, 4), did not display enhanced migration to CCR2 receptor ligands used at different concentrations (Figure 6A-C). On the contrary, TAP-2–deficient and healthy donor–derived CANK lines migrated similarly to the CXCR3 ligand, interferon-inducible protein of 10 kDa (IP-10; Figure 6D). This result further supports the notion that the accelerated responsiveness of TAP-2–deficient CANK cells to CCR2 receptor ligands was not the result of a generalized alteration in CANK cell responsiveness to chemoattractants but was specific to stimulation through the CCR2 pathway.
TAP2-deficient CANK cell lines display specific enhanced migration ability to CCR2 ligands. Migration assays were performed, as described in “Materials and methods.” Dose-dependent migration capacity of healthy donor (▪) CANK cell lines and TAP-2–deficient CANK cells (♦) to various concentrations of MCP-1 (A), MCP-2 (B), MCP-3 (C), and IP-10 (D) was examined. In each experiment, the migration index of TAP-2–deficient CANK cells from all wells with a certain chemokine concentration were averaged and presented in the graph. Healthy-donor–derived CANK-cell migration indeces (obtained from 7 healthy donors and the patient's mother) were averaged and grouped similarly. **P < .01 by Student t test. Error bars indicate SD. Results are of 1 representative experiment of 3 experiments performed on CANK cell lines generated on 3 independent occasions from each donor.
TAP2-deficient CANK cell lines display specific enhanced migration ability to CCR2 ligands. Migration assays were performed, as described in “Materials and methods.” Dose-dependent migration capacity of healthy donor (▪) CANK cell lines and TAP-2–deficient CANK cells (♦) to various concentrations of MCP-1 (A), MCP-2 (B), MCP-3 (C), and IP-10 (D) was examined. In each experiment, the migration index of TAP-2–deficient CANK cells from all wells with a certain chemokine concentration were averaged and presented in the graph. Healthy-donor–derived CANK-cell migration indeces (obtained from 7 healthy donors and the patient's mother) were averaged and grouped similarly. **P < .01 by Student t test. Error bars indicate SD. Results are of 1 representative experiment of 3 experiments performed on CANK cell lines generated on 3 independent occasions from each donor.
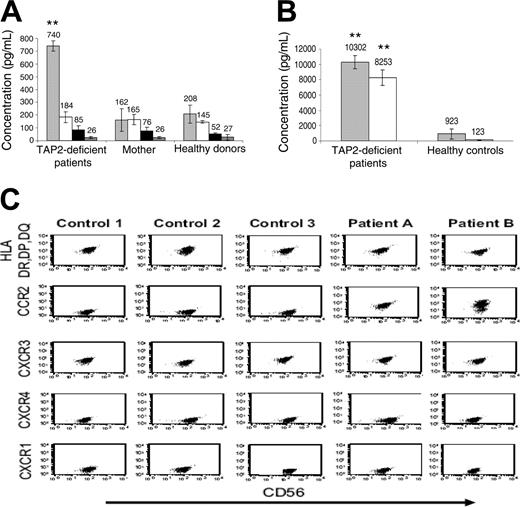
In vivo aberrant expression of CCR2 receptor on chronically activated NK cells in patients with TAP-2 deficiency
A potentially informative means for evaluating the role and involvement of certain chemokines in undergoing systemic immune responses is to measure their levels in the serum.32 Therefore, we examined serum levels of different chemokines in blood samples obtained from healthy donors and from family members with TAP-2 deficiency. Surprisingly, compared with those of the patients' mother and 23 unrelated healthy donors, MCP-1 levels were significantly and consistently elevated in 3 different serum samples obtained independently from each of the patients with TAP-2 deficiency (Figure 7A). No such alteration was observed in serum levels of ligands for chemokine receptors CXCR4, CXCR3, and CCR7 (stromal-derived factor 1 [SDF1], IP-10, and SLC, respectively).
To extrapolate our results, we checked for IL-2 and MCP-1 abundance in BAL samples obtained from patients A and B and compared them with those obtained from 5 donors without any known pathologic pulmonary conditions. Remarkably, both cytokines were up-regulated in BAL samples from patients A and B by more than 100-fold (Figure 7B). This result demonstrates that the necessary requirements for induction and stimulation of the CCR2 pathway on NK cells are present in patients with TAP-2 deficiency in vivo. Indeed, when characterizing the phenotype of CD56+CD3– NK cells purified from the cellular fractions from the BAL samples of patients A and B and 3 immunosuppressed patients with ongoing lung inflammation, we obtained in vivo verification for our results. Remarkably, BAL-derived activated NK cells (expressed high levels of NK activation marker [MHC class 2]) from patients A and B, but not from the control donors, expressed high levels of CCR2 chemokine receptor (Figure 7C). No differences were observed in the expression of other chemokine receptors examined (CXCR1, CXCR3, and CXCR4) between the 2 subgroups (Figure 7C). It is also important to note the remarkable correlation between chemokine receptor expression results obtained in vitro (Figures 2, 3) and in vivo (Figure 7C) on the chronically activated NK cells of TAP-2–deficient patients and control donors, further supporting the validity of our results.
Discussion
NK cells, like other innate immune effector cells, continuously patrol different organs through extensive arrays of chemokine receptors expressed on their surfaces.13,18,22 Different receptors have been implicated in dictating the accumulation of distinct NK subsets to various organs: (1) CXCR3 and CCR7 regulate NK-cell homing to lymph nodes21,33 ; (2) CXCR4 regulates mouse NK cells homing to spleen and bone marrow20 ; (3) CCR1 and CXCR3 control NK trafficking to inflamed liver.20 After encountering tumor or virally infected cells or homing to inflammatory sites, NK cells become activated through stimulation by locally secreted cytokines and specific recognition of ligands by their activating lysis receptors.6 Such interactions carefully regulate specific changes in the chemokine receptor repertoire for several possible reasons. First, certain receptors can be down-regulated to reduce NK-cell capability to leave the inflammatory site and to prevent the overstimulation of certain chemokine receptor–mediated migration pathways. Second, NK cells can up-regulate certain chemokine receptors, such as CXCR3 and CCR4, that can be involved in lymphocyte retention and in the control of specific localization of such cells within the inflammatory site.34 Indeed, it has been suggested that stromal expression of CXCR3 ligands in the deciduae14 and the inflamed liver35 results in the active retention of NK cells in these organs.
Recent literature has formulated the hypothesis that activated NK cells represent a double-edged sword in human TAP deficiency by participating in immune defense against pathogens and by demonstrating some damaging capabilities toward normal tissues and contributing to the progression of autoimmune lung fibrosis at later stages of disease.4,36 Unexpectedly, in spite of the systemic down-regulation of MHC class 1 molecules, immediate and severe NK-cell attack does not occur at early stages of disease.4,10 Several groups3,4,10,11 have added useful pieces to this puzzle; multiple mechanisms allowing NK cells from TAP-2–deficient patients to be tolerant, at least to some extent and under certain conditions, to MHC class 1–deficient autologous cells have been discovered. These mechanisms generally include the down-regulation of certain activating receptors and the up-regulation of inhibitory receptors, especially CEACAM1, which is involved in MHC class 1–independent inhibition of NK-cell activation.37
However, in some patients with TAP-2 deficiency, these fail-safe mechanisms become insufficient to maintain immune tolerance, and those patients experience chronic granulomatous lesions in the respiratory tract and skin, closely mimicking Wegener granulomatosis syndrome.3,7 In depth analysis of these lesions made the possibility of chronic infectious agents as a cause for these symptoms unlikely because the patients were unresponsive to diverse aggressive antibiotic and tuberculostatic drugs. Furthermore, the observation that these lesions were a result of massive infiltration and aggregation of activated NK cells and were partially responsive to steroid agents supported the possibility that they were caused by a dysregulated accumulation of autoreactive activated NK cells.7 Molecular mechanisms potentially underlying these modifications in chronically activated NK-cell accumulation and retention in such lesions are still unknown.
Analysis of NK cells and cytokines in serum and bronchioalveolar lavage samples from patients with TAP-2 deficiency. (A) Serum samples obtained from patients A, B, and C, their mother, and 9 healthy donors were analyzed by ELISA assays for the detection of MCP-1 (▦), SDF1 (□), IP10 (▪), and secondary lymphoid tissue chemokine (SLC; ▩) chemokines. Results are of 1 representative experiment of 3 experiments performed on serum samples obtained on 3 independent occasions from each donor. (B) MCP-1 (▦) and IL-2 (□) levels in BAL samples obtained from patients A and B were compared with those in BAL samples obtained from 5 controls without underlying pulmonary disease. (C) Purified NK cells from BAL samples obtained from patients A and B were compared with those of BAL samples obtained from 3 immunosuppressed patients with sustained lung infection and inflammation and were analyzed for the expression of HLA-DR, DP, DQ, CCR2, CXCR3, CXCR4, and CXCR1 receptors. ** P < .001 by Student t test. Error bars indicate SD.
Analysis of NK cells and cytokines in serum and bronchioalveolar lavage samples from patients with TAP-2 deficiency. (A) Serum samples obtained from patients A, B, and C, their mother, and 9 healthy donors were analyzed by ELISA assays for the detection of MCP-1 (▦), SDF1 (□), IP10 (▪), and secondary lymphoid tissue chemokine (SLC; ▩) chemokines. Results are of 1 representative experiment of 3 experiments performed on serum samples obtained on 3 independent occasions from each donor. (B) MCP-1 (▦) and IL-2 (□) levels in BAL samples obtained from patients A and B were compared with those in BAL samples obtained from 5 controls without underlying pulmonary disease. (C) Purified NK cells from BAL samples obtained from patients A and B were compared with those of BAL samples obtained from 3 immunosuppressed patients with sustained lung infection and inflammation and were analyzed for the expression of HLA-DR, DP, DQ, CCR2, CXCR3, CXCR4, and CXCR1 receptors. ** P < .001 by Student t test. Error bars indicate SD.
Given the plethora of candidate chemoattraction-regulating molecules mediating cell-trafficking pathways that can potentially contribute to the aberrant recruitment and retention of chronically stimulated NK cells in some patients with TAP-2 deficiency, we applied a general screening method for such targets by performing high-output proteomic analysis of NK-membrane–enriched fractions derived from a healthy donor (mother) and patient B. Strikingly, this analysis highlighted the aberrant expression of CCR2 chemokine receptor on TAP-2-deficient CANK cells that was further verified and functionally characterized in all 3 patients, as described. The impressive ability of mass spectrometry–based proteomics to identify proteins from increasingly complex mixtures is a driving force for new scientific approaches. Current proteomic technologies still face a transient deficit in sensitivity, robustness and widely accessible tools for systematic handling and analysis of the output.38 Nevertheless, their ability and advantage in supplying new “leads” is invaluable. Many of the interesting proteins expressed in activated NK (ANK) cells, such as Notch3, Killer-cell immunoglobulin-like receptor of 2 domains, long cytoplasmic tail X [KIR2DLX], D-prohibitin, and multiple high-scoring hypothetic proteins (see Supplemental Tables S1 and S2), are currently being studied by our group but are beyond the scope of this paper.
CCR2 chemokine receptor plays a distinctive role in the recruitment of certain mononuclear subsets by interacting with monocyte chemotactic proteins (MCPs) 1, 2, 3, and 4.39 The spectrum of action of these chemokines encompasses dendritic, T, CD56bright, NK, and immature B cells and, most prominently, monocytes and macrophages.40 Interestingly, CCR2-mediated interaction has been extensively shown to regulate several lung fibrosis– and granuloma formation–associated abnormalities.41,42 For example, in bronchiolitis obliterans syndrome, which is an autoimmune syndrome characterized by persistent peribronchiolar leukocyte infiltration occurring mainly after lung transplantation leading to airway fibrosis and obliteration, and in bleomycin-induced interstitial pulmonary fibrosis models, CCR2 signaling has been shown to play a fundamental role in the promotion of lung injury.43,44
Granulomas are characterized histologically by a prominent nodular collection of macrophages with occasional admixture of epithelioid cells and multinucleate giant cells. Remarkably, CCR2 has also been proven to act as a crucial regulator in the formation of pulmonary45 and hepatic granulomas.46 MCP-1/CCR2 interactions were shown to carefully regulate the number, size, and progression of such lesions in several models by manipulating macrophage homing and microarchitectural positioning in these lesions. Moreover, in Mycobacterium tuberculosis infection, chronic interaction with this pathogen induces the activation of macrophages, and subsequently CCR2 expression on these cells facilitates their recruitment and organization in these discrete lesions laced in a network of matrix proteins.47 These granulomas represent an important defense mechanism against such infectious organisms. CCR2-deficient mice fail to develop proper granulomatous responses on infection with Mycobacterium because of the improper migration capabilities of monocytes.48
In light of these observations, it is tempting to suggest an analogy between NK cells in patients with TAP-2 deficiency and activated macrophages in patients with chronic inflammatory lung disease. NK cells in patients with TAP-2 deficiency are exposed to sustained activation, which is projected to occur in the context of recurrent infections and, more important, of chronic inflammation because of the relative reduction of inhibitory signals derived from MHC class 1–recognizing receptors (eg, KIRs, LIR).2,3 Subsequently, the aberrant induction of CCR2 receptor on these chronically activated NK cells might alter their trafficking capabilities and local positioning within the inflammatory site and implicate them in granuloma lesion formation. The significant in vivo expression of CCR2 on chronically activated NK cells from BAL samples and the up-regulation of IL-2 and MCP-1 in the lungs and bronchioles of patients with TAP-2 deficiency strengthens the possibility that the required inflammatory milieu for functional CCR2 expression on NK cells is present in vivo.
A recent study49 has shown that CCR1 can influence NK-cell content in pulmonary granuloma lesions in mice; however, CCR1 did not influence the granuloma formation process or lesion size. Our analyses did not point out any aberrant expression of this receptor on NK cells in patients with TAP-2 deficiency (Figures 2, 3). Interestingly, CCR2 has also been shown to mediate the migration of immune cells (eg, Langerhans cells) to the inflamed skin by the local production of chemokine ligands for this receptor.50 These observations could implicate CCR2-mediated interactions in the homing of TAP-2-deficient CANK cells to inflammatory lesions in the skin.7 CCR10 chemokine receptor is another important player in immune-cell recruitment to the inflamed skin.51 However, RT-PCR analysis of CCR10 expression and functional migration to its ligand, CCL27, did not highlight any differences between the derived ANK cells of patients with TAP-2 deficiency and of healthy donors (data not shown).
Molecular mechanisms linking MHC class 1 deficiency and the various phenotypic alterations in receptor expression on the TAP-2–deficient CANK-cell surface are unknown. Alterations to NK-cell development, attributed to the unique MHC class 1 low-expressing microenvironment, have been suggested as the potential explanation for some of these unique characteristics.4 However, a certain extent of phenotypic heterogeneity has been described among the few patients with TAP-2 deficiency described thus far. For instance, down-regulation of natural cytotoxicity receptors was not observed in 2 patients with TAP-2 deficiency described by Vitale et al,3 implying that dissimilar mutations causing TAP-2 deficiency or different environmental factors could also affect the CANK-cell phenotype in these patients. The limited number of diagnoses of this rare syndrome and the major obstacles to studies on human-obtained tissue samples have slowed down and limited the ability of researchers to provide answers.
In summary, we have presented data emphasizing the fundamental concept of regulation of chemokine receptor expression on immune effector cells at different stages of the immune response. Similar to the augmented expression of CCR6 receptor on Langerhans cells in Langerhans-cell histiocytosis,9 the aberrant expression of certain receptors on CANK cells—as was the case for CCR2 receptor in patients with TAP-2 deficiency—can be implicated in the pathologic trafficking and retention of these cells at inflammatory sites and the subsequent propagation of fibrosis and autoimmunity.
Prepublished online as Blood First Edition Paper, July 21, 2005; DOI 10.1182/blood-2005-03-0855.
Supported by research grants from the Israel Cancer Research Foundation (O.M.), the Israel Science Foundation (O.M.), the European Commission (QLK-CT-2002-011112; O.M.), the Hadassah Women's Health Center (O.M.), and the Fritz Thyssen Foundation (O.M.).
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Amnon Peled, Ori Wald, Gal Markel, and Roi Gazit for helpful discussions and excellent assistance.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal