Our understanding of the pathogenesis of antiphospholipid syndrome is incomplete but in this issue, 2 papers, by Kuwana and colleagues and de Laat and colleagues, give significant new insights into the mechanisms underlying the generation of antiphospholipid antibodies as well as their heterogeneity and the significance of this in relation to thrombotic disease.
The paradox of lupus anticoagulant (LAC) antibodies, which prolong phospholipid-dependent clotting times in vitro but are linked in vivo to thrombosis and to pregnancy failure, has been the subject of extensive speculation and experimentation for over 3 decades. It is now becoming clear that lupus anticoagulants are members of a family of antibodies that share the property of reacting with anionic phospholipids including cardiolipin. In many cases, the relevant epitopes reside not on phospholipids themselves but on a plasma protein with affinity for negatively charged phospholipid. β2–Glycoprotein I (β2GPI) is one such protein, a member of the family of complement control proteins (CCPs) present in plasma at a high concentration. Its crystal structure has been solved: it has 5 domains characterized by CCP repeats, the first 4 being regular repeats and the fifth includes a cluster of positively charged amino acids responsible for binding to anionic phospholipids. We know now that some LACs are β2GPI dependent while others bind different proteins, notably prothrombin. It is also known from observational studies in patients that among antiphospholipid antibodies, LACs associate more strongly with thrombosis than do anti-cardiolipin antibodies, and immunoglobulin G (IgG) antibodies associate with thrombosis more strongly than do IgM antibodies. Finally, and most recently, it has been shown that it is the β2GPI-specific LACs that are most clearly linked to a history of thrombosis in subjects with systemic lupus erythematosus (SLE).1 Importantly, IgG from serum containing antiphospholipid antibody is pathogenic in animal models of thrombosis and pregnancy failure.2,3 The pathogenesis of thrombosis in antiphospholipid syndrome appears to involve several mechanisms, including inhibition of the protein C anticoagulant pathway and activation of cells including monocytes and endothelial cells. Tantalizingly, it has been demonstrated recently that an additional pathogenic mechanism may explain the link between early pregnancy loss and antiphospholipid antibodies: activation of complement through the classical pathway.4 FIG1
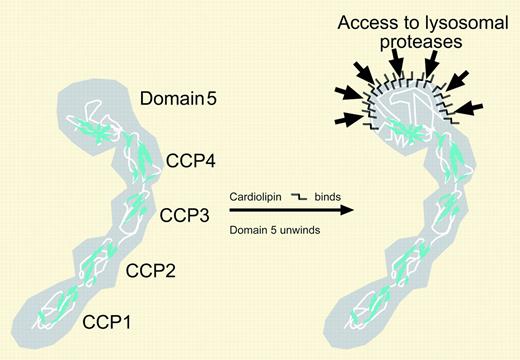
β2–glycoprotein I is shown as a space-filling representation with polypeptide backbone highlighted. On binding anionic phospholipid, domain 5 undergoes steric change so that cryptic epitopes are unmasked in the lysosomes of antigen-presenting cells. The antibodies thought to be important in mediating thrombosis are directed against domain 1.
β2–glycoprotein I is shown as a space-filling representation with polypeptide backbone highlighted. On binding anionic phospholipid, domain 5 undergoes steric change so that cryptic epitopes are unmasked in the lysosomes of antigen-presenting cells. The antibodies thought to be important in mediating thrombosis are directed against domain 1.
The “anticoagulant” effect of LACs in vitro is most likely explained by competition for binding to anionic phospholipid between the coagulation factors of prothrombinase and β2GPI or prothrombin due to increased affinity of these last 2 proteins for the catalytic surface as a result of complex formation with anti-β2GPI or antiprothrombin, respectively. This results in impairment of thrombin generation and lengthening of the time to clot.5
Two important reports in the current issue advance still further our understanding of these important antibodies. There has been controversy over the domain of the β2GPI molecule involved in binding of pathogenic antibodies. de Laat and colleagues demonstrate conclusively that it is antibodies directed against an epitope containing Gly40 and Arg43 in domain 1 that have LAC activity and associate strongly with thrombosis, unlike heterogeneous antibodies that bind elsewhere on the molecule. But how are these autoantibodies generated? The report by Kuwana and colleagues offers novel insights into this process. A popular concept to explain why autoreactive lymphocytes are so commonly detected in the absence of disease is that they recognize “cryptic” epitopes. When antigen is taken up by antigen-presenting cells, it is degraded by a series of specific proteases, regulators, and specialized chaperonins6 so that only a subset of possible epitopes are displayed to interrogating lymphocytes. Cryptic epitopes bind with high affinity to major histocompatibility complex (MHC) class II but are not usually part of the repertoire displayed on the surface of antigen-presenting cells. Kuwana et al show that only β2GPI bound to phospholipids can be presented successfully to autoreactive clones. Antiphospholipid antibodies are commonly present in chronic inflammatory disease, such as SLE, but also after acute illness including some infections. In both situations there may be increased circulating phospholipids derived from apoptotic cells7 or pathogens. The phospholipids are then postulated to “reveal” β2GPI to pre-existing autoreactive T-cell clones, allowing autoantibody formation. The process of epitope spreading must then be invoked in the extension of autoantibodies from the domain V epitopes highlighted in the study of Kuwana et al to those directed against domain 1 and thereby thrombosis, as highlighted by de Laat et al. Lupus “anticoagulant” and thrombosis are not so paradoxical after all. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal