Comment on Barker et al, page 1343
In this issue, Barker and colleagues at the University of Minnesota report stem cell transplantation procedure outcomes in 23 adults and adolescents with high-risk hematologic malignancies, treated with fully ablative conditioning prior to infusion of 2 partially HLA-matched unrelated cord blood units.
Clinical reports outlining transplantation procedure outcomes for adults undergoing umbilical cord blood (UCB) transplantation point to a 10% to 15% incidence of primary graft failure and delayed time to hematopoietic recovery. UCB graft nucleated cell dose has been noted to correlate both with time to attain donor myeloid engraftment and event-free survival in myeloablated patients infused with single-unit grafts.1 These clinical observations have set the stage for intensive ongoing clinical and laboratory research focused on strategies to foster UCB allogeneic donor engraftment, thereby allowing wider application of this immune tolerant stem cell source for adults requiring allogeneic transplantation.
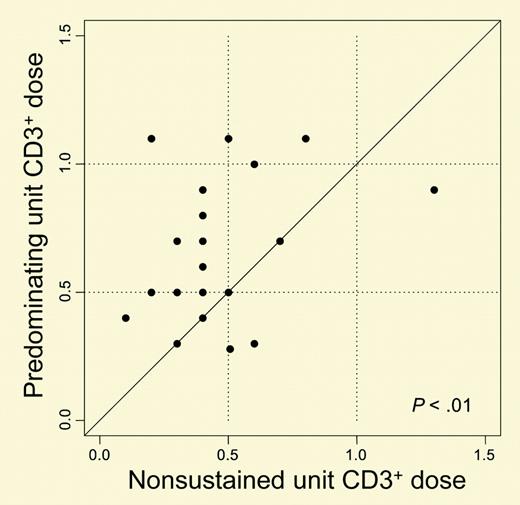
In this issue, Barker and colleagues at the University of Minnesota report stem cell transplantation procedure outcomes in 23 adults and adolescents with high-risk hematologic malignancies, treated with fully ablative conditioning prior to infusion of 2 partially HLA-matched unrelated cord blood units. Median age in this series was 24 years (range, 13-53 years). Each patient received 2 HLA-mismatched UCB units thawed and infused without prior ex vivo expansion. Median combined graft nucleated cell dose was 3.5 × 107/kg (range, 1.1 × 107/kg to 6.3 × 107/kg). All evaluable patients (n = 21) engrafted neutrophils at a median of 23 days (range, 15-41 days). At the time of myeloid engraftment, chimerism revealed the presence of both UCB donors in some patients, with emergence of one UCB unit predominating in all patients by day 100. The authors examined graft characteristics possibly predictive of UCB unit predominance and found that neither nucleated or CD34+ graft cell dose nor HLA match was predictive. Importantly, however, the predominating UCB unit had a significantly higher CD3+ graft lymphocyte cell dose (P < .01; see figure). Further observations outlined in this issue parallel that reported in other reports that use of unrelated cord blood is associated with a low incidence of acute graft-versus-host disease (GVHD) and that event-free survival approximates that observed in the unrelated setting after infusion with adult donor marrow and peripheral blood stem cell grafts.FIG1
Comparison of the infused CD3+ dose of the unit predominating in donor engraftment (y-axis) versus the nonsustained unit (x-axis). See the complete figure in the article beginning on page 1343.
Comparison of the infused CD3+ dose of the unit predominating in donor engraftment (y-axis) versus the nonsustained unit (x-axis). See the complete figure in the article beginning on page 1343.
There are preliminary reports summarizing donor engraftment after infusion of more than one UCB unit into adult patients with intent to provide increased hematopoietic stem cell dose.2 The results of these reports indicate that in most instances “in vivo” selection occurs and only one UCB unit engrafts long-term. There does not appear to be crossed immunologic rejection when 2 HLA-disparate UCB grafts are infused, albeit with graft selection criteria including minimum HLA 4/6 match to the patient as well as between the 2 infused grafts. Graft characteristics of importance in allogeneic transplantation with conventional bone marrow and peripheral blood stem cell grafts include cell dose and HLA matching.3-5 The effect of the number and type of HLA disparities on engraftment after UCB transplantation has not been fully elucidated. While there is delayed hematopoietic recovery in recipients of UCB compared with conventional bone marrow and peripheral blood stem cell grafts, it is remarkable that engraftment occurs at all, considering that there are at least a log less nucleated and CD34 cell doses.4,5 UCB grafting is unique in allogeneic transplantation in that it is the only graft routinely infused into recipients who are HLA disparate at more than one HLA loci, without requirement for T/natural killer (T/NK) lymphocyte depletion. Since mechanisms for the graft-facilitating activity of donor lymphocytes include inhibition or elimination of residual recipient immune cells capable of mediating graft rejection, 6 HLA disparity may therefore serve to augment rather than reduce successful UCB engraftment in the host. These graft immune factors may be of particular importance in the setting of adult UCB transplant recipients who receive further reduced nucleated and CD34 graft cell doses compared with pediatric recipients. These clinical results reported by Barker et al therefore support the hypothesis that UCB donor engraftment is determined not only by graft CD34 content but also by graft T-lymphocyte number. Further studies are warranted to determine the impact of HLA-matching loci and graft cell dose thresholds (> 2 × 107/kg) on unrelated donor UCB stem transplantation procedure outcomes in adults. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal