Three papers published in this issue of Blood provide important insights into the pathogenesis of juvenile hemochromatosis. Two papers identify novel mutations in the genes encoding hemojuvelin and hepcidin, respectively, while the third shows a direct of hepcidin upon iron uptake by gut epithelial cells.
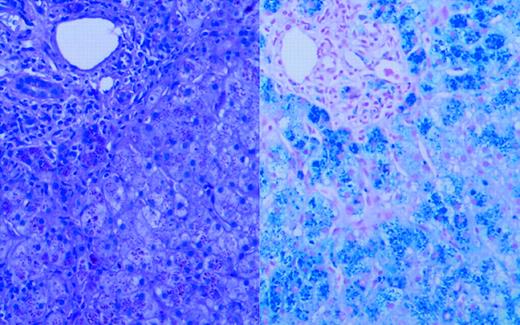
Juvenile hemochromatosis (JH) is a genetically heterogeneous, autosomal-recessive disorder of iron transport and storage. This rare condition is associated with accumulation of parenchymal iron in the second and third decades of life as a consequence of increased gastrointestinal absorption and decreased macrophage storage, and leads to iron-associated cardiac disease, hypogonadotropic hypogonadism, diabetes, and arthropathy.1 FIG1
Liver biopsy. See the complete figure in the article beginning on page 2176.
Liver biopsy. See the complete figure in the article beginning on page 2176.
Many patients with JH have disease linked to chromosome 1q. The chromosome 1q–associated JH gene has recently been cloned and is called HFE2 or HJV; its protein product is called hemojuvelin. Mutations in this gene have been shown to be associated with the JH phenotype.2 In addition, loss-of-function mutations in the HAMP gene, which encodes the liver protein hepcidin, also have been shown to be associated with the JH phenotype.3 These papers extend these findings and suggest possible linkages between hemojuvelin and hepcidin that may account for the development of JH.
Huang and colleagues describe a novel mutation in HJV that results in a premature termination codon at position 321 of the hemojuvelin protein, leading to truncation of the protein prior to its putative transmembrane domain. They also report a missense mutation in cis in the hemojuvelin signal peptide, although this mutation may be functionally insignificant. The proband in their study also expressed a previously described missense mutation (I281T) in HJV.2 The coexpression of the HJV mutations presumably caused loss of function of the hemojuvelin protein and led to severe parenchymal iron overload by the age of 19 years in this patient.
In the second paper, Matthes and colleagues describe 2 Portuguese siblings with JH who are homozygous for a previously unreported mutation in the 5′-untranslated region (UTR) of the HAMP gene, which results in a new initiation codon and a frame shift leading to the production of an abnormal protein. No normal hepcidin could be detected in the patients' urine. Both siblings also were heterozygous for the H63D mutation in the HFE1 gene, although it seems unlikely that this increased the severity of the JH phenotype. The very different clinical presentations of the 29-year-old proband and his 24-year-old sister, despite possessing the same HFE1 and HAMP mutations, suggest the existence of additional modifying features that affect the expression of the iron overload phenotype.
In the third paper, Yamaji and colleagues describe a direct inhibitory effect of hepcidin on iron uptake in vitro by human intestinal epithelium Caco-2 cells. Hepcidin decreases apical iron uptake and decreases expression of iron-responsive element-regulated form of divalent metal transporter 1 (DMT1[+IRE]) mRNA and protein levels but has no effect on iron efflux and iron-regulated gene 1 (IREG1) expression. These studies have several limitations, not least that the naturally occurring concentrations of hepcidin in biologic fluids are largely unknown; these investigators used an arbitrary concentration of 10 μM and did not show dose-response kinetics. Similarly, the hepcidin preparation used in their studies included a number of different hepcidin species, and it is unclear which are active form(s).
Where do these studies lead? Studies in genetically modified mice and clinical observations in humans suggest that hepcidin plays a key role in the physiologic regulation of iron storage. Overexpression of hepcidin (eg, in states of chronic inflammation) leads to an iron-unresponsive anemia that resembles the anemia of chronic disease. Conversely, genetic deficiencies of hepcidin lead to JH.4
Hemojuvelin is the other key player in this scenario. The majority of characterized cases of JH have involved mutations in HJV/hemojuvelin, yet the function of this gene remains unknown. Hepcidin levels are decreased in patients with HJV mutations;2 loss-of-function mutations in hepcidin lead to JH; and HJV- and HAMP-associated JH are clinically indistinguishable. It is therefore tempting to speculate that hemojuvelin and hepcidin are linked in a common pathway that regulates iron storage. Hemojuvelin would regulate the levels of hepcidin, the latter being the key effector protein in iron storage. The studies of Yamaji et al suggest a mechanism by which hepcidin may regulate iron uptake by intestinal epithelial cells. However, considerable further work will be necessary to confirm such a pathway and to define the physiologic mechanisms that control iron uptake and storage. The relationship between hemojuvelin/hepcidin and the HFE1 pathway responsible for late-onset Northern European hereditary hemochromatosis also will need to be established. Finally, it will be necessary to define genetic and nongenetic modifiers of iron accumulation to account for the observed wide variation in JH clinical phenotype.5 ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal