Abstract
Short microvilli cover the surfaces of circulating mammalian lymphocytes. The surfaces of monocytes and neutrophils are very different, containing ruffles as their predominant structure. In this study, we present the first quantitative characterization of lymphocyte microvilli. From analysis of scanning electron micrographs, we find that median microvillar length and surface density range from 0.3 to 0.4 μm and 2 to 4 microvilli/μm2, respectively, on lymphocytes from a variety of sources. As with similar structures from other cells, lymphocyte microvilli contain parallel bundles of actin filaments. Lymphocyte microvilli rapidly disassemble when exposed to the actin-sequestering molecule, Latrunculin A. This disassembly parallels cellular actin filament depolymerization and is complete within 2 minutes, suggesting that lymphocyte microvilli undergo continuous assembly and disassembly. In contrast to previous reports suggesting lymphocyte microvillar density to be reduced on lymphocytes from Wiskott-Aldrich syndrome (WAS) patient, we find no such deficiency in either mouse or human WAS protein (WASp)–deficient lymphocytes. These results suggest that WASp is either not involved in or is redundant in the rapid dynamics of lymphocyte microvilli.
Introduction
Cell surfaces are rarely flat and generally contain a variety of protrusions and/or invaginations. Microvilli are fingerlike protrusive structures found on the surfaces of many cells and are abundant on the surfaces of circulating T and B lymphocytes.1 While definitive roles for lymphocyte microvilli have not been established, a proposed function is in segregation of surface receptors during extravasation.2 Two receptors involved in the initial rolling phase of extravasation, L-selectin3,4 and α4β7 integrin,5 localize to microvillar tips. In contrast, the β2 integrins that mediate subsequent stable adhesion and diapedesis localize to nonprotrusive regions of the cell surface.5 This spatial segregation of surface receptors might enable a temporal segregation of adhesive function during extravasation. Lymphocytes expressing chimeric L-selectin constructs that no longer localize to microvilli do not roll on L-selectin ligands,3 supporting this hypothesis. Microvilli are correlated with metastatic potential of certain cancers,6 perhaps due to their role in extravasation. In addition, receptors for HIV, including CD4, CC chemokine receptor 5, and CXC chemokine receptor 4, localize to microvilli,7 suggesting a potential role for microvilli in HIV infection.
Other fingerlike protrusions on cell surfaces, including epithelial microvilli and surface-attached filopodia on many cell types, depend on actin filaments for their structure.8,9 These filaments are organized in parallel bundles that appear to span the length of the microvillus and are cross-linked to each other and to the microvillar membrane by a number of proteins.10 The dynamics of these structures vary immensely. While filopodia grow and shrink intermittently by alternate assembly and disassembly of their actin filaments,11 epithelial microvilli maintain relatively constant length. Nevertheless, the actin filaments in epithelial microvilli constantly turn over the actin monomer subunits by a balance between addition of new monomers at the distal tip and release of monomers at the base.12
While lymphocyte microvilli also appear to be actin dependent,3 details of their structure and dynamics are unknown. Also unknown are the mechanisms by which lymphocyte microvilli are assembled. Possible clues to this issue, however, are data suggesting microvillar number to be reduced on lymphocytes from patients with the Wiskott-Aldrich syndrome (WAS) immunodeficiency disease.13-16 The defective protein in this disease is Wiskott-Aldrich syndrome protein (WASp),17 a hematopoietic-lineage molecule and an activator of the actin nucleation factor, Arp2/3 complex.18 These findings suggest a pathway wherein WASp induction of Arp2/3 complex–mediated actin filament assembly enables microvillar formation.
An as-yet-unanswered question in this model is how Arp2/3 complex, which causes formation of short, branched filaments, could mediate formation of long, parallel actin filaments found in microvilli. In migrating adherent melanoma cells, Arp2/3 complex appears to mediate filopodial formation indirectly through its role in generating the leading edge lamellipodium.19 After Arp2/3 complex generates branched filaments, some of these filaments are bundled and elongated, causing filopodia to protrude out of the lamellipodium. However, blood lymphocytes are not adherent and contain no recognizable lamellipodia or ruffles, raising doubts as to whether their microvilli could assemble through a similar mechanism.
In this study, we examine lymphocyte microvilli in detail using a quantitative scanning electron microscopy (SEM) assay. The data reveal that lymphocytes from human blood and mouse blood, as well as from a murine B-lymphoma culture line, possess similar microvillar surfaces. These microvilli are highly dynamic, disassembling within 2 minutes when treated with the actin monomer sequestering drug, Latrunculin A (LatA). The actin filaments in lymphocyte microvilli are arranged in parallel bundles and are the major actin-based structures in these cells. Lymphocytes from several patients with severe WAS and from WASp-deficient mice display microvillar characteristics similar to those of normal lymphocytes. It therefore appears that development of these structures on the lymphocyte cell surface can occur in the absence of WASp activity.
Materials and methods
Cells used
Human lymphocytes were isolated from healthy volunteers (Committee for the Protection of Human Subjects [CPHS] 15406) under sterile conditions. One unit of blood was drawn by venous puncture into acid citrate dextrose (ACD), and mixed with Dextran T-500 (Amersham, Piscataway, NJ) to 2% in a separatory funnel to aggregate erythrocytes. After 30 minutes, the lower erythrocyte layer was drained and the upper layer was centrifuged for 10 minutes at 300g max in a swinging bucket rotor (same centrifugation conditions used for subsequent steps unless indicated). The supernatant was removed, and the pellet was resuspended in 30 mL iced lysis buffer (8.3 g/L NH4Cl, 1 g/L NaHCO3, 0.04 g/L disodium EDTA [ethylenediaminetetraacetic acid]) and incubated on ice for 5 minutes. All subsequent steps were carried out on ice or at 4° C. Cells were centrifuged and then washed 2 × in 300 mL 0.9% NaCl. The washed pellet was brought to 30 mL in 0.9% NaCl; then 5 mL was layered carefully onto 7 mL Ficoll-Paque (Amersham) in six 15-mL polypropylene tubes (Fisher, Pittsburgh, PA). These step gradients were centrifuged at 400g max for 15 minutes in a swinging bucket rotor. The interfaces between NaCl solution and Ficoll were carefully removed, pooled, diluted 5-fold in RPMI1640 + glutamine (Invitrogen, Frederick, MD), and centrifuged. After 2 washes in RPMI, cells were resuspended to 1 × 106/mL in medium (RPMI + 10% fetal bovine serum [FBS; HyClone defined; HyClone, Logan, UT]), plated onto 10-cm–diameter tissue culture plates, and incubated for 1 hour at 37° C/5% CO2. Nonadherent cells were centrifuged, resuspended in medium, and plated on tissue culture plastic a second time. Nonadherent cells from the second plating were pelleted, resuspended at 1 × 106/mL in prewarmed medium, and incubated at 37° C/5% CO2 for 1 hour before experimentation.
Preparations isolated in this manner contained 85% to 90% lymphocytes by forward- and side-scatter analysis in a FACSCalibur (Becton Dickinson, San Jose, CA), the remainder being mostly smaller cells (erythrocytes, platelets, and broken cells, 3%-5%), aggregates (1%-2%), polymorphonuclear leukocytes (PMNs; 1.5%-2.5%), and monocytes (2%-3%). Using fluorescently labeled antibodies and flow analysis (FACSCalibur), and gating out the smallest particles, cells were 88% to 93% T lymphocytes (CD3+), 2% to 3% B lymphocytes (CD19), 2% to 3% neutrophils (CD66b), and 0% to 1% monocytes (CD14).
Lymphocytes from severe human WAS patients and control subjects were isolated by Ficoll-Hypaque gradient followed by plating onto tissue culture plastic to remove adherent monocytes. Isolated lymphocytes were flash-frozen in liquid nitrogen and fixed in glutaraldehyde after thawing. Mutations were as follows: patient 1, deletion of bases 107 and 108 of open reading frame, resulting in a premature STOP at amino acid 36; patient 2, 121C>T, resulting in R41stop; patient 3, 291G>A, resulting in R86H; and patient 4, undetermined. The presence of WASp in these lymphocytes was not examined. All patients had clinically diagnosed severe WAS.
Human neutrophils (PMNs) were recovered from the pellets of Ficoll gradients during lymphocyte isolation, washed 3 × in RPMI, suspended to 1 × 106/mL in medium, and incubated for 1 hour at 37° C/5% CO2. This fraction contained 80% to 85% neutrophils by fluorescent antibody or light scattering flow analysis (FACSCalibur), with less than 1% lymphocytes or monocytes.
Human monocytes were isolated by counter-current elutriation.20 The final cell population was suspended to 1 × 106/mL in medium and incubated for 1 hour at 37° C/5% CO2.
Mouse lymphocytes were isolated from C57Bl/6 mice (normal lymphocytes) or from the WASp knock-out (KO) strain (WASp–/– lymphocytes21 ). Blood was drawn by cardiac puncture from mice killed by CO2 asphyxiation. A lymphocyte/monocyte population was isolated using Lympholyte-Mammal (Cedarline Laboratories, Hornby, ON, Canada). Monocytes were removed by plating on tissue culture plastic, as described for human lymphocytes. The final cell population was suspended to 1 × 106/mL in medium and incubated for 1 hour at 37° C/5% CO2.
The 300.19 cell line (Abelson-transformed murine pre-B lymphoma) was obtained from Dr Geoffrey Kansas (Northwestern Medical School, Chicago, IL) and cultured in RPMI1640 + 10% FBS + 0.05 mM 2-mercaptoethanol. For experiments, cells were used at 0.5 to 1 × 106/mL.
Scanning electron microscopy
Cells were fixed in suspension from medium at 37° C/5% CO2. Cells (150 μL) were added to 1.35 mL room temperature fixative (3.5% glutaraldehyde [EM Sciences, Fort Washington, PA] in 100 mM NaPO4 [pH 7.4]) and rapidly mixed by inversion. After 2 hours of fixation, cells were centrifuged in a swinging bucked rotor at 300g max for 5 minutes. The pellet was washed twice in 1.5 mL NaPO4 (pH 6.0), then resuspended in less than 20 μL of this buffer. This drop of cells was placed on top of a 5-mm round acid-washed glass coverslip (EM Sciences) previously coated with 0.1% poly-l-lysine (> 300 000 molecular weight [MW]; Sigma, St Louis, MO). After 30 minutes (while serenaded by a selection of baritone arias), cells on the coverslip were treated with 0.5 mL fixative for 30 minutes. Coverslips were postfixed in 0.5% osmium tetroxide for 1 hour, dehydrated in graded ethanol washes followed by hexamethyldisilazane (HMDS; Aldrich), desiccated overnight under vacuum, mounted onto 12-mm round aluminum SEM stubs (EM Sciences), and gold-palladium sputter coated. Coverslips were viewed on a Zeiss DSM 962 scanning electron microscope (Carl Zeiss, Thornwood, NY) at 10 kV and 10-mm working distance.
Microvillar quantification from SEM images
Low-magnification images (× 1000 or × 2000) were used to characterize cell populations by morphology. Cells classified as possessing microvilli had no apparent large or small ruffles. Microvilli were distinguished from small ruffles by their appearance as fingerlike projections on cell sides. “Damaged” cells were pockmarked or were missing large areas of plasma membrane. Platelets, red blood cells, and reticulocytes were readily discernable. High-magnification images (× 10 000 or × 20 000) of individual cells were used for measuring microvillar lengths and densities, using NIH Image software (NIH, Bethesda, MD). A 2 × 2 μm (1 × 1 μm for mouse lymphocytes) box was created on top of the cell. The number of microvilli that originated in the box was counted to determine microvillar density. Individual microvilli within the box were traced to determine microvillar length. Images were manipulated using Photoshop (Adobe, San Jose, CA).
Light and fluorescence microscopy
Cells were fixed in suspension from medium at 37° C/5% CO2 in all cases. Cells (150 μL) were added to 1.35 mL fixative (4% formaldehyde/0.05% glutaraldehyde in phosphate-buffered saline [PBS]), mixed by inversion, and fixed for 1 hour at 23° C. After washing twice in PBS, 100 μL cells was spotted onto 12-mm round acid-washed coverslips coated with 0.1% poly-l-lysine and incubated at 23° C for 30 minutes. Fixative (1 mL) was added to coverslip and incubated for 15 minutes, followed by several PBS washes. Cells were treated with 0.1 μM tetramethylrhodamine isothiocyanate (TRITC)–phalloidin (Sigma) in PBS with 1% calf serum and 0.1% saponin for 1 hour at room temperature, then washed several times in PBS and mounted in PVA/DABCO (Prolong Anti-Fade; Molecular Probes, Eugene, OR). A Zeiss Axioplan2 microscope (Carl Zeiss) with × 100, 1.4 NA Plan-Apochromat objective was used. Hamamatsu (Bridgewater, NJ) C4742-98 cooled CCD camera and OpenLab software (Improvision, Lexington, MA) were used to collect a Z-series (0.5-μm Z-sections). OpenLab software was used to deconvolve the Z-series. Images were manipulated using Photoshop (Adobe, San Jose, CA).
Transmission electron microscopy (TEM)
Cells were fixed in suspension from medium at 37° C/5% CO2. Cells (1 mL) were added to 9 mL fixative (2.2% glutaraldehyde in 100 mM NaPO4 [pH 7.4]) and fixed for 2 hours. Cells were postfixed in 1% osmium tetroxide, stained en-bloc with 0.5% uranyl acetate in water, dehydrated in a graded ethanol series, embedded, and thin sectioned. Sections were stained with 2% uranyl acetate in methanol for 20 minutes, followed by lead citrate for 5 minutes, and then viewed on a JEOL 2000FX transmission electron microscope (JEOL USA, Peabody, MA). Images were manipulated using Photoshop (Adobe, San Jose, CA).
Cellular polymerized actin quantification
Cellular polymerized actin was quantified using TRITC-phalloidin following published methods.22 Briefly, a known number of cells was fixed in suspension with 4% formaldehyde/0.05% glutaraldehyde in PBS for 1 hour, washed in PBS several times, permeabilized with 1% TritonX-100 in PBS for 5 minutes, stained with 1 μM TRITC-phalloidin in PBS with 1% bovine serum albumin for 1 hour, washed in PBS several times, and extracted in 1 mL of 100% methanol overnight. The TRITC-phalloidin in the methanol extract was quantified in an ISS PC1 spectrofluorometer (ISS, Champaign, IL) at 546-nm excitation and 577-nm emission. A standard curve was created from known concentrations of TRITC-phalloidin. Cytoplasmic volume was calculated as described in the next paragraph.
Lymphocyte surface area and volume calculations
Surface area and cytoplasmic volume of human blood lymphocytes were calculated by assuming radii of 2.7 and 1.5 μm, respectively, for the cell and nucleus (measured from light, scanning, and transmission electron micrographs). For 300.19 cells, these values are 4 and 2.5 μm. From these values, the volume and surface area of human lymphocytes, assuming they are spherical, are 6.83 × 10–14 L and 92 μm2, respectively. Our measured microvillar density (4.1 per μm2; Table 2) means that human lymphocytes possess on average 377 microvilli. Assuming a cylindric shape for microvilli, with average radius of 50 nm and height of 380 nm (Table 2), the volume and surface area of single microvilli are 2.98 × 10–18 L and 0.119 μm2, respectively. Total microvillar volume and surface area are 1.12 × 10–15 L and 45 μm2, respectively. These values cause a 1.6% increase in cytoplasmic volume, and a 49% increase in cell surface area.
Microvillar parameters of lymphocytes
Cells . | Median microvillar length, μm . | Length standard deviation (n) . | Microvillar density, villi/μm2 . | Density standard deviation (n) . |
|---|---|---|---|---|
| 300.19 cells | 0.39 | 0.27 (1267) | 2.9 | 1.3 (27) |
| Human lymphs | 0.38 | 0.22 (1200) | 4.1 | 1.2 (28) |
| Mouse lymphs | 0.31 | 0.14 (310) | 4.1 | 1.0 (19) |
| Mouse WASp KO | 0.31 | 0.16 (227) | 3.3 | 1.6 (17) |
| Human healthy control | 0.30 | 0.11 (212) | 4.4 | 2.1 (6) |
| Human WAS 1 | 0.29 | 0.13 (404) | 6.4 | 1.0 (6) |
| Human WAS 2 | 0.30 | 0.15 (277) | 4.8 | 0.7 (7) |
| Human WAS 3 | 0.31 | 0.10 (277) | 5.6 | 1.4 (7) |
| Human WAS 4 | 0.30 | 0.10 (396) | 4.0 | 1.5 (11) |
Cells . | Median microvillar length, μm . | Length standard deviation (n) . | Microvillar density, villi/μm2 . | Density standard deviation (n) . |
|---|---|---|---|---|
| 300.19 cells | 0.39 | 0.27 (1267) | 2.9 | 1.3 (27) |
| Human lymphs | 0.38 | 0.22 (1200) | 4.1 | 1.2 (28) |
| Mouse lymphs | 0.31 | 0.14 (310) | 4.1 | 1.0 (19) |
| Mouse WASp KO | 0.31 | 0.16 (227) | 3.3 | 1.6 (17) |
| Human healthy control | 0.30 | 0.11 (212) | 4.4 | 2.1 (6) |
| Human WAS 1 | 0.29 | 0.13 (404) | 6.4 | 1.0 (6) |
| Human WAS 2 | 0.30 | 0.15 (277) | 4.8 | 0.7 (7) |
| Human WAS 3 | 0.31 | 0.10 (277) | 5.6 | 1.4 (7) |
| Human WAS 4 | 0.30 | 0.10 (396) | 4.0 | 1.5 (11) |
Human healthy control indicates human lymphocytes prepared in the same manner as WAS lymphocytes; human WAS 1 to 4, lymphocytes from WAS patients.
Results
Microvilli are the predominant cell surface feature on lymphocytes
We used scanning electron microscopy (SEM) to examine the surface morphologies of human and mouse blood lymphocytes. Our intent was to examine blood lymphocytes in suspension after little prior manipulation to minimize cell surface alterations.
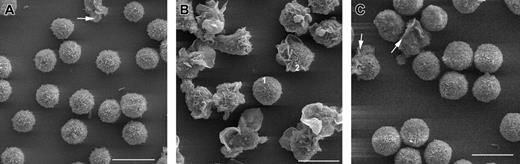
Viewed by SEM at low magnification, most cells from human or mouse lymphocyte preparations (85% and 90%, respectively) are spherical and display short microvilli (Figures 1A and 2A-B; Table 1). A small proportion (11% for human and 7% for mouse) is elongated and contains large membrane ruffles. A low percentage of cells appears “damaged” (perforated or missing areas of plasma membrane) and very low percentages of readily identifiable erythrocytes or platelets are present. As observed previously,23 mouse lymphocytes (2.5-3 μm diameter) are significantly smaller than are those from humans (5-6 μm).
Low-magnification SEM of cells from human blood. (A) Lymphocytes. Arrow indicates cell with surface ruffles. (B) Monocytes. Cell 1 displays no ruffles but has microvilli. Cell 2 displays ruffles on one half and microvilli on the other. (C) PMNs. Arrows indicate cells with large ruffles. Scale bars are 10 μm.
Low-magnification SEM of cells from human blood. (A) Lymphocytes. Arrow indicates cell with surface ruffles. (B) Monocytes. Cell 1 displays no ruffles but has microvilli. Cell 2 displays ruffles on one half and microvilli on the other. (C) PMNs. Arrows indicate cells with large ruffles. Scale bars are 10 μm.
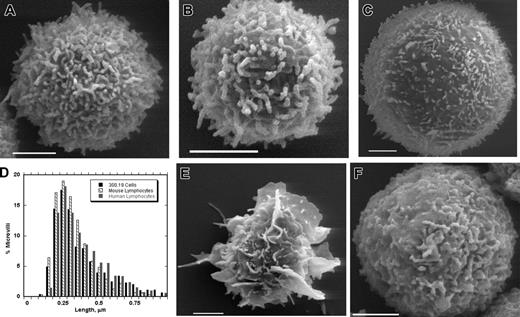
Surface morphologies of white blood cells. SEMs of a human blood lymphocyte (A), mouse blood lymphocyte (B), 300.19 murine pre-B lymphoma cell (C), human blood monocyte (E), and human blood PMN (F). Scale bars represent 2 μm. (D) Histogram of microvillar lengths for 300.19 cells (▪), mouse blood lymphocytes (▧), and human blood lymphocytes (▦). Bins are 0.05 μm. Numeric data are in Table 1.
Surface morphologies of white blood cells. SEMs of a human blood lymphocyte (A), mouse blood lymphocyte (B), 300.19 murine pre-B lymphoma cell (C), human blood monocyte (E), and human blood PMN (F). Scale bars represent 2 μm. (D) Histogram of microvillar lengths for 300.19 cells (▪), mouse blood lymphocytes (▧), and human blood lymphocytes (▦). Bins are 0.05 μm. Numeric data are in Table 1.
Low-magnification (× 2000) SEM characterization of white blood cells
Cell type . | No. of cells . | % villi . | % small ruffles . | % large ruffles . | % smooth . | % RBCs . | % platelets . |
|---|---|---|---|---|---|---|---|
| Human lymphs | 1382 | 85 | 0 | 11 | 3 | 0 | 2 |
| Human PMNs | 774 | 0 | 77 | 20 | 2.5 | 0 | 1 |
| Human monos | 120 | 13 | 0 | 84* | 3 | 0 | 2 |
| Mouse lymphs | 174 | 90 | 2 | 7 | 0 | 1 | 0 |
| 300.19 cells | 325 | 84 | 0 | 0 | 16 | — | — |
Cell type . | No. of cells . | % villi . | % small ruffles . | % large ruffles . | % smooth . | % RBCs . | % platelets . |
|---|---|---|---|---|---|---|---|
| Human lymphs | 1382 | 85 | 0 | 11 | 3 | 0 | 2 |
| Human PMNs | 774 | 0 | 77 | 20 | 2.5 | 0 | 1 |
| Human monos | 120 | 13 | 0 | 84* | 3 | 0 | 2 |
| Mouse lymphs | 174 | 90 | 2 | 7 | 0 | 1 | 0 |
| 300.19 cells | 325 | 84 | 0 | 0 | 16 | — | — |
RBCs indicates red blood cells; PMN, polymorphonuclear leukocytes (neutrophils); monos, monocytes; and —, not applicable.
Of these cells, 62% had at least one obvious microvillus.
In contrast to lymphocyte preparations, enriched fractions of monocytes or PMNs have very different surface characteristics. Most cells in monocyte preparations (84%) contain large ruffles as their predominant surface feature (Figures 1B and 2E; Table 1). These cells often display microvilli along with these large ruffles, and sometimes microvilli are embedded in the ruffles. Most cells in the PMN preparations display short ruffles throughout their surface (Figures 1C and 2F; Table 1) and no readily identifiable microvilli. About 20% of the cells in the PMN preparations are elongated and highly ruffled at one end.
We used high-magnification SEM images (Figure 2) to quantify both microvillar length and microvillar surface density on individual lymphocytes, selecting cells at random for this analysis. Despite differences in cell diameter (about 5.5 μm for human lymphocytes and 2.5 μm for mouse lymphocytes), both microvillar parameters are similar between species (Table 2), with median microvillar lengths of 0.3 to 0.4 μm and densities of 3 to 4 microvilli/μm2. Neither population was sorted by lymphocyte class, with the human pool being 90% T lymphocyte and 3% B lymphocyte, and the mouse pool being 63% T lymphocyte and 32% B lymphocyte (“Materials and methods”). Even so, the cell-to-cell variation in microvillar parameters is small, suggesting that T and B cells have similar surface morphologies.
We also examined microvillar features on 300.19 murine pre-B lymphoma cells, a line used extensively for studies of adhesion receptors and cell rolling.4 These cells, although significantly larger than either primary lymphocyte (8.2-μm median diameter), possess microvillar parameters similar to those of primary B and T cells (Table 2). The length distributions of microvilli on lymphocytes from these 3 cell types are also largely similar (Figure 2D).
Lymphocyte microvilli are dynamic, actin-dependent structures
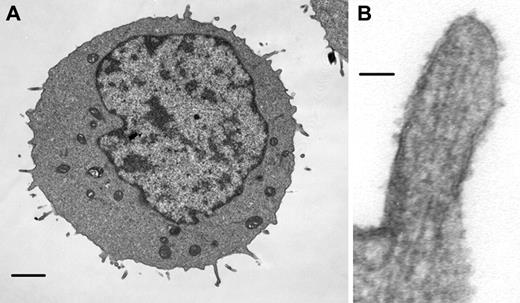
Other fingerlike surface structures, such as epithelial microvilli and growth cone filopodia, are dependent on long parallel bundles of actin filaments,8,9 and past studies of lymphoma cell microvilli suggest that they are actin dependent since they disassemble after a 30-minute treatment with high concentrations of cytochalasin D.3 We examined the actin dependence of lymphocyte microvilli in more detail. Transmission electron microscopy demonstrates that 300.19 cell microvilli contain parallel assemblies of filaments of similar diameter to actin filaments (Figure 3). Fluorescence microscopy of these cells, using the fluorescently labeled actin filament-binding molecule, phalloidin, reveals intense staining at the cell periphery and in microvillar protrusions (Figure 4A-B). Similar staining is observed in human blood lymphocytes (not shown). This staining suggests that microvilli are the major actin filament-containing structures in lymphocytes, since no ruffles or stress fibers are readily visible.
Lymphoma cell microvilli contain parallel actin filaments. Transmission electron micrographs of a 300.19 cell (A) and of an individual 300.19 cell microvillus (B). Note parallel striations in microvillus, which have diameters similar to those of actin filaments. Scale bars represent 1 μm (A) and 50 nm (B).
Lymphoma cell microvilli contain parallel actin filaments. Transmission electron micrographs of a 300.19 cell (A) and of an individual 300.19 cell microvillus (B). Note parallel striations in microvillus, which have diameters similar to those of actin filaments. Scale bars represent 1 μm (A) and 50 nm (B).
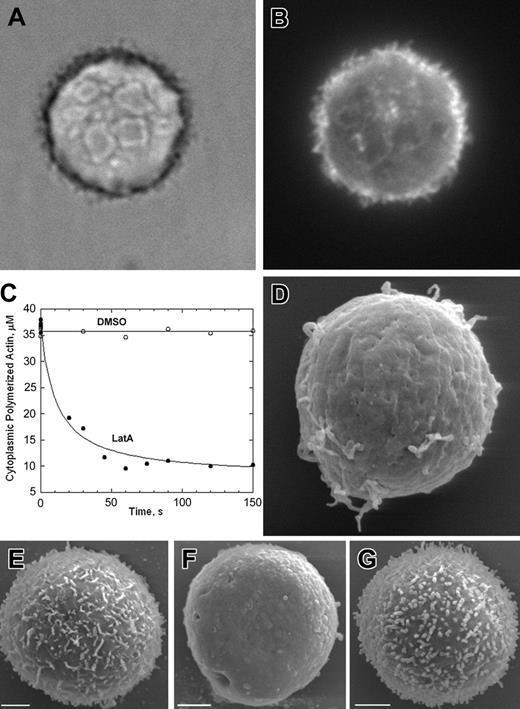
Lymphoma cell microvilli are dynamic and actin dependent. (A) Phase-contrast micrograph of a fixed 300.19 cell. (B) Rhodamine fluorescence of same 300.19 cell stained with rhodamine-phalloidin. (C) Time course of decrease in cellular rhodamine-phalloidin after treating 300.19 cells with 1 mm LatA or with dimethyl sulfoxide (DMSO) carrier. (D) SEM of 300.19 cell 2 minutes after treatment with 1 μM LatA. (E-G) SEMs of 300.19 cells before treatment (E), after 10 minutes in 1 μM LatA (F), and 30 minutes after LatA wash out (G). Scale bars are 2 μm. Original magnification × 1000 (A-B) and × 10 000 (D).
Lymphoma cell microvilli are dynamic and actin dependent. (A) Phase-contrast micrograph of a fixed 300.19 cell. (B) Rhodamine fluorescence of same 300.19 cell stained with rhodamine-phalloidin. (C) Time course of decrease in cellular rhodamine-phalloidin after treating 300.19 cells with 1 mm LatA or with dimethyl sulfoxide (DMSO) carrier. (D) SEM of 300.19 cell 2 minutes after treatment with 1 μM LatA. (E-G) SEMs of 300.19 cells before treatment (E), after 10 minutes in 1 μM LatA (F), and 30 minutes after LatA wash out (G). Scale bars are 2 μm. Original magnification × 1000 (A-B) and × 10 000 (D).
The actin monomer-binding small molecule, Latrunculin A (LatA), prevents actin monomer addition to filaments.24 Since dynamic cellular actin filaments rapidly gain and lose monomers from their ends,25 LatA causes depolymerization of dynamic filaments by blocking polymerization, but affects stable filaments much less rapidly. When added to 300.19 cells, LatA causes cellular polymerized actin levels to drop by 75% within 1 minute (Figure 4C). Surface microvilli disappear on a similar timescale (Figure 4D). Upon LatA washout, microvilli recover on a slower timescale (Figure 4E-G), possibly reflecting the high affinity of LatA for monomers. These results demonstrate that microvilli are highly dynamic, growing and shrinking on a timescale of seconds to minutes.
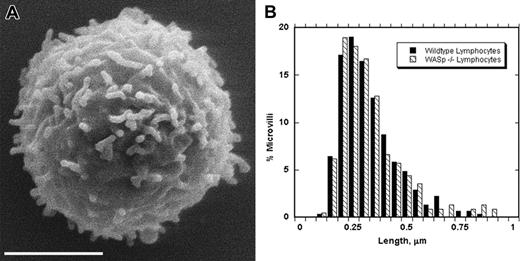
Lymphocyte microvilli are not affected by lack of WASp
Previous studies using circulating lymphocytes or immortalized T lymphocytes from human WAS patients suggested that WASp deficiency resulted in decreased lymphocyte microvillar density and altered morphology.13-15 Another study using splenic B cells from WASp knock-out mice suggested a similar phenotype.16 We analyzed circulating lymphocytes from WASp knock-out mice using our quantitative SEM assay. Surprisingly, we found no difference in microvillar length and only a slight (20%) decrease in microvillar density (Figure 5; Table 2).
Lymphocytes from WASp knock-out mice have normal microvilli. (A) SEM of representative blood lymphocyte from WASp knock-out mouse. Scale bar represents 2 μm. (B) Histogram comparing microvillar lengths for wild-type and WASp knock-out mouse lymphocytes. Bins are 0.05 μm. Numeric data are in Table 2.
Lymphocytes from WASp knock-out mice have normal microvilli. (A) SEM of representative blood lymphocyte from WASp knock-out mouse. Scale bar represents 2 μm. (B) Histogram comparing microvillar lengths for wild-type and WASp knock-out mouse lymphocytes. Bins are 0.05 μm. Numeric data are in Table 2.
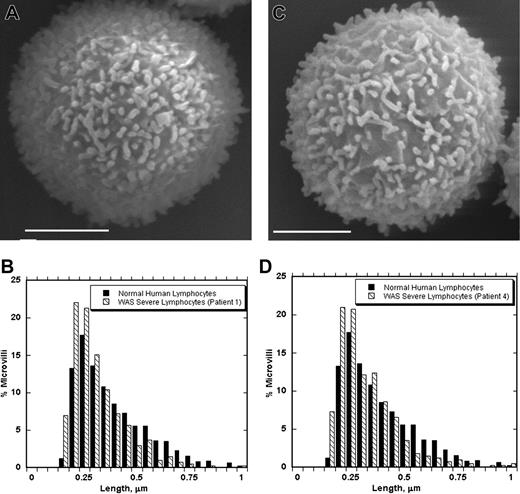
We also obtained lymphocyte preparations from 4 different human patients clinically diagnosed as displaying severe WAS. The genotypes of 3 patients had been determined. There are 2 patients who are predicted to express no WASp, since they possess mutations resulting in premature stop codons at amino acids 36 and 41, respectively. The third patient contains a missense mutation resulting in R86H, an acknowledged mutational hot spot that has been identified as causing severe WAS in other patients.17 Lymphocyte microvillar lengths and densities from all patients were indistinguishable from those of healthy subjects isolated by the same procedure (Figure 6; Table 2).
Lymphocytes from human severe WAS patients have normal microvilli. (A,C) SEMs of representative blood lymphocytes from 2 patients with severe WAS. Scale bars represent 2 μm. (B,D) Histograms comparing microvillar lengths from normal human lymphocytes and those from the respective WAS patient. Bins are 0.05 μm. Numeric data are in Table 2.
Lymphocytes from human severe WAS patients have normal microvilli. (A,C) SEMs of representative blood lymphocytes from 2 patients with severe WAS. Scale bars represent 2 μm. (B,D) Histograms comparing microvillar lengths from normal human lymphocytes and those from the respective WAS patient. Bins are 0.05 μm. Numeric data are in Table 2.
Discussion
In this study, we present the first quantitative characterization of lymphocyte microvilli. These short (300-400 nm) structures are abundant (3-4 per μm2) on the surfaces of lymphocytes from several sources. From our measurements, microvilli increase the surface area of human blood lymphocytes appreciably (49%), while having little effect on cytosolic volume (1.6% increase; “Materials and methods”). In addition to preferential localization of rolling receptors to microvilli,3-5 this increase in surface area might enhance the ability of these cells to roll.
Previous publications using TEM suggested that both monocytes and PMNs possessed surface microvilli.26-28 Other work using SEM revealed that PMNs expressed ruffles predominantly on their surface29,30 and pointed out that distinguishing between microvilli and ruffles by TEM was difficult. Due to the small sizes of the protrusions on PMNs and lymphocytes, we are not able to declare definitively that PMNs possess ruffles exclusively or that lymphocytes do not possess any ruffles. However, our work suggests that the dominant surface protrusions on lymphocytes are microvilli, while those on PMNs are predominantly ruffles. The protrusions on monocytes are much larger and are predominately ruffles with some microvilli interspersed.
While both microvilli and ruffles are actin dependent, these structures differ greatly in their actin filament architecture and the proteins that mediate these architectures. Ruffles contain a meshwork of short filaments cross-linked in an end-to-side manner, these cross-links being mediated by Arp2/3 complex and filamin.31 In contrast, the long, parallel filament bundles in microvilli are cross-linked side-to-side by proteins such as fimbrin, villin, fascin, and espins.10 These architectural differences strongly suggest major differences in regulation of assembly/disassembly of these structures, so to consider them equivalent would be erroneous. However, L-selectin localizes both to microvillar tips on lymphocytes and to ridges of ruffles on PMNs,3,4,29 so the 2 structures might be functionally equivalent in this respect.
The small size of lymphocyte surface protrusions makes it difficult to test whether lymphocytes contain some small ruffles in addition to microvilli or if PMNs contain microvilli embedded in their small ruffles. Resolution of this question will be critical to determining assembly mechanisms for these structures. Recent studies on filopodia in melanoma cells, which contain parallel filaments like microvilli, suggest that filopodial filaments might be generated from within a substantial rufflelike actin filament network. Short filaments generated by Arp2/3 complex in this network are bundled by the cross-linking protein, fascin, and elongate to form filopodia.19 From our SEM and TEM images, no comparable extensive actin filament network exists in lymphocytes, but we cannot rule out the possibility that a more modest network serves the same purpose.
The rapid retraction of microvilli upon LatA treatment suggests that these structures are highly dynamic, growing and shrinking on a timescale of seconds to minutes. LatA sequesters actin monomers but does not actively depolymerize filaments. Thus, lymphocyte microvilli must constantly cycle between assembly and disassembly, driven by polymerization and depolymerization of actin filaments. When LatA blocks polymerization, filaments depolymerize due to normal depolymerization mechanisms. Their dynamics suggest that lymphocyte microvilli are able to adapt rapidly to signals. Such structures might be more widespread than is generally appreciated, as several cell types appear to possess short, dynamic microvilli.32
Our results suggest that WASp deficiency in either mouse or human lymphocytes does not result in dramatic microvillar length or density defects in circulating lymphocytes. These findings differ from data published previously in several reports,13-16 which may reflect differences in cell preparative techniques in the different studies. One study used SEM to examine allo-specific T lymphocytes isolated from WAS patient blood and cultured for several months in the presence of interleukin-2 (IL-2)– and mitomycin C–treated Raji cells.14 As major changes to T-cell cytoskeleton occur upon T-cell activation, and WASp plays an important role in this process,21,33 this latter finding may reflect features of activated rather than unstimulated T cells. Similarly, published data on microvillar structure on splenic B cells from WASp KO mice involved analysis of cells treated with lipopolysaccharide or with anti-CD40 and IL-4.16 One other report on lymphocyte microvillar structures from WAS patients did involve analysis of peripheral lymphocytes isolated and prepared in a similar manner to those in our work.13 However, the WAS gene had not been identified at that time and molecular characterization of the patients was not possible. Moreover, the microvillar defects observed in that study were mild, and the data may not substantively differ from our results.
In summary, WASp does not appear crucial for maintaining microvillar morphology on lymphocytes. One possible explanation for these findings is that WASp effects on microvillar actin filaments can be achieved through other effector pathways as well. The recently identified actin assembly abilities of formin proteins34 suggest some redundancies between formins and WASp functions and raise the possibility that formins compensate for WASp in microvillar regulation. Similarly, N-WASP activity may also compensate for the absence of WASp in relation to modulating microvillar dynamics. Alternately, WASp may be more relevant in activated cells, just as WASp effects on immunologic synapse formation arise only in the context of T-cell receptor engagement.21,33 Resolving these issues will require further investigation into the effectors that localize to microvillar structures and definition of the extent to which WASp effects on actin remodeling overlap with effects of other cytoskeletal modulatory proteins.
Prepublished online as Blood First Edition Paper, May 6, 2004; DOI 10.1182/blood-2004-02-0437.
Supported by the Norris Cotton Cancer Center American Cancer Society Institute grant IRG-82-003-18, by a Pew Biomedical Scholars grant, and by the National Institutes of Health (NIH) grant P20RR16437 from the Centers of Biomedical Research Excellence (COBRE) Program of the National Center for Research Resources (H.N.H.). Also supported by a grant from the Canadian Institutes of Health Research (CIHR) and a CIHR Senior Scientist Award (K.A.S.); and grants from the Deutsche Forschungsgemeinschaft (SFB413, GRK 438), Friedrich Baur Stiftung, and August Lenz Stiftung (S.L.). K.A.S. is a Canadian Institutes of Health Senior Scientist.
An Inside Blood analysis of this article appears in the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We are greatly indebted to the WAS patients and their families for contributing to these studies. We also thank Peter Morganelli (VA Hospital, White River Junction, VT) and Paul Wallace (formerly at Dartmouth Medical School, now at Roswell Park Cancer Center) for contributing purified monocytes; Dr Charles Daghlian and Louisa Howard in the Ripple Electron Microscope Facility at Dartmouth for their expertise and advice; Duane Compton and his laboratory for use of his fluorescence microscope and lots of advice; Peter C. Weber for continuous support; and Barbara Boehlig for technical support.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal