Comment on Munitic et al, page 4165
The tight regulation of the interleukin-7 receptor (IL-7R) during T-cell development occurs so that developing pro- and pre-T cells are uniquely poised to use limited IL-7, especially after the initial wave of T-cell production.
Signaling through the IL-7R is essential for thymic production of T lymphocytes as it promotes the survival and T-cell receptor (TCR) rearrangements of “double-negative” pro- and pre-T cells.1 The expression of IL-7R is very tightly regulated on thymocytes. Essentially all double-negative thymocytes express the IL-7R, but its expression is extinguished as cells transit to the CD4+CD8+ stage, where selection occurs, followed by reinduction on “single-positive” mature thymocytes.2
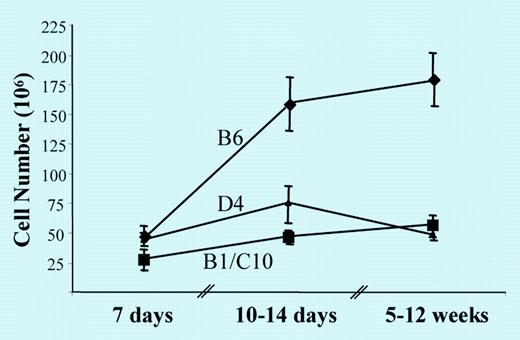
The study of Munitic and colleagues in this issue of Blood address the question of why it is necessary to down-regulate IL-7R expression on CD4+CD8+ thymocytes. This issue was examined by evaluating the consequences of aberrant thymic expression of a transgenic IL-7R, such that virtually all thymocytes were IL-7R+. The main observation from multiple founder lines was that transgenic IL-7R expression led to a decrease in thymic cellularity that was evident early in life (see figure).
Age-dependent changes in IL-7Rα Tg thymus. See the complete figure in the article beginning on page 4165.
Age-dependent changes in IL-7Rα Tg thymus. See the complete figure in the article beginning on page 4165.
These investigators went on to show that thymic negative selection of IL-7R transgenic thymocytes in fetal thymic organ culture was normal after stimulation with anti-TCR antibodies or with nominal antigen. These data tend to rule out that the reason the IL-7R is normally down-regulated at the double-positive stage is to maintain proper selection. Furthermore, in chimeric mice that received an equal number of normal and transgenic bone marrow cells, the reconstituted thymus was much smaller than found for mice that received only wild-type bone marrow, but the ratio of wild-type to IL-7R transgenic thymocytes remained approximately 1:1. This experiment indicates that improper expression of the transgenic IL-7R did not result in an intrinsic defect in developing thymocytes.
So why does an IL-7R transgenic thymus contain fewer thymocytes, even in the presence of wild-type cells? Careful analysis of the transgenic thymus revealed that there was a large decrease in the number of precursor CD4-CD8- cells that were arrested in their development and were prone to apoptosis with lower Bcl-2 levels. This phenotype is analogous to the few double-negative thymocytes found in IL-7R-deficient mice. The transgenic pre-T cells, therefore, behaved as if they were starved of IL-7. Importantly, the provision of IL-7 to developing IL-7R transgenic thymocytes increased thymus cellularity. Thus, it appears that the relatively large number of double-positive thymocytes that inappropriately expressed the transgenic IL-7R used most of the IL-7, such that little was available for precursor double-negative cells, adversely affecting thymopoiesis.
Over the years there has been much emphasis concerning the outcome of cytokine receptor signal transduction with downstream biologic responses. An important implication of this work is that a normal developmental response leading to the correct number of mature T cells critically depends upon tight regulation of expression of the IL-7R on thymocytes and secretion of appropriate levels of IL-7 by stromal cells. As many receptors use overlapping signal transduction pathways, the availability of a cytokine and the proximity of cells that express the respective receptor, as shown for IL-7 and the IL-7R, may represent an important component that contributes to cytokine specificity in vivo.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal