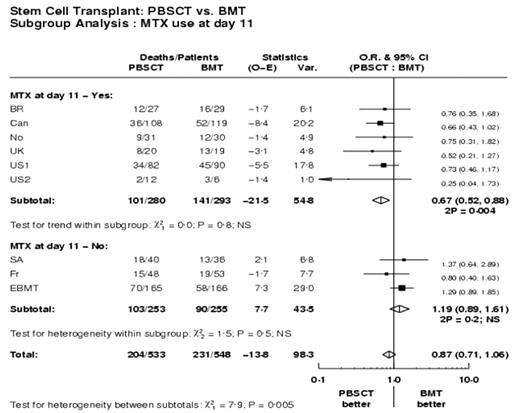
We conducted an IPDMA using data from 9 randomized trials comparing allogeneic PBSC transplants to bone marrow (BM), focusing specifically on the issue of the administration of 3 vs. 4 doses (day 11) of MTX as part of a regimen for GVHD prophylaxis which included cyclosporine. The administration of day 11 MTX was trial specific and data were analysed by intention to treat, irrespective of whether the 4th dose of MTX was actually given. Six trials containing 573 patients prescribed 4 doses of MTX while 3 trials containing 508 patients prescribed 3 doses of MTX. Four doses of MTX conferred a statistically significant survival advantage, death odds ratio (OR) 0.67 (CI 0.52–0.88) (p=0.0036) for recipients of PBSC compared to BM, while with 3 doses, there was no statistically significant difference. The difference between the two subgroups was significant (test of interaction chi2=7.9;p=0.005). Disease-free survival was also significantly better among recipients of PBSC in the 4 dose studies OR 0.62 (CI 0.48–0.80) while no difference was seen in the 3 dose studies. Test of interaction between the two subgroups was significant, chi2=9.7;p=0.002. The effect on survival and DFS appeared to be due primarily to the rates of relapse. In the 4-dose studies relapse rates were 36.6% at 6 years among recipients of BM compared to 19.2% among recipients of PBSC (p=0.0015). The rates of relapse in the 3 dose studies were 26% for both recipients of PBSC and BM. Test of interaction between the two subgroups was again significant (chi2=4.3; p=0.04). Thus the administration of 4 doses of MTX had a negative impact among recipients of BM which resulted in higher relapse rates. The effect on relapse-related mortality was also significant, 23.6% BM v. 14.2 % PBSC (p=0.018) in the 4 dose studies but not significant in 3 dose subgroup (14 vs. 23%, p=0.42). Test of interaction between the two subgroups was not significant (chi2=0.7;p=0.4). The effect was not due to non-relapse mortality which was not statistically different among patients in the 4-dose MTX studies and the 3 dose MTX studies. The rates of acute GVHD grades 2–4 were the same among recipients of PBSC or BM in both the 4 dose and 3 dose studies. Chronic extensive GVHD was higher among recipients of PBSC irrespective of whether patients received 3 or 4 doses of MTX; at 5 years 57.3% PBSC v. 47.3% BM, (p=0.0037) for 4 dose, 49.2% PBSC v. 26.1% BM, (p=0.00004). Both platelet and neutrophil engraftment was faster in PBSC arm (p<0.0001), but interestingly the test of interaction between two subgroups was significant only for platelet engraftment (chi2=11.4;p=0.0007) and not for neutrophil engraftment (chi2=0.6;p=0.4). We conclude that 4 doses of MTX given as part of a GVHD prophylaxis regimen was beneficial for the most important patient outcomes (survival, DFS and relapse) for patients receiving allogeneic PBSC but detrimental to recipients of BM. We hypothesize that the 4th dose of MTX provided extra immunosuppression among BM recipients resulting in a reduced anti-leukemic effect. This theory should be tested in a prospective randomized study.
Skip Nav Destination
Oral Sessions|
November 16, 2004
The Administration of Day 11 Methotrexate (MTX) for GVHD Prophylaxis Improves Outcomes for Patients Receiving Allogeneic Peripheral Blood Stem Cell Transplantation (PBSC) : An Individual Patient Data Meta-Analysis (IPDMA) from the Stem Cell Trialists Collaborative Group. Free
William I. Bensinger, MD
William I. Bensinger, MD
1Division of Oncology, Fred Hutchinson Cancer Research Center, University of Washington, Seattle, WA, USA.
Search for other works by this author on:
Blood (2004) 104 (11): 621.
Citation
William I. Bensinger; The Administration of Day 11 Methotrexate (MTX) for GVHD Prophylaxis Improves Outcomes for Patients Receiving Allogeneic Peripheral Blood Stem Cell Transplantation (PBSC) : An Individual Patient Data Meta-Analysis (IPDMA) from the Stem Cell Trialists Collaborative Group.. Blood 2004; 104 (11): 621. doi: https://doi.org/10.1182/blood.V104.11.621.621
Download citation file:
November 16 2004
Advertisement intended for health care professionals
Cited By
Advertisement intended for health care professionals

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal