Abstract
The efficacy of allogeneic hematopoietic stem-cell transplantation (allo-HSCT) for NK-cell neoplasms is unknown. We investigated the results of allo-HSCT for NK-cell neoplasms between 1990 and 2003 through questionnaires. A hematopathologist reclassified the pathological diagnoses according to the WHO classification. Of 345 patients from 76 hospitals who underwent allo-HSCT for malignant lymphoma, 32 had NK-cell neoplasms: extranodal NK/T-cell lymphoma (n=27), blastic NK-cell lymphoma (n=3), and aggressive NK-cell leukemia (n=2). Fifteen were chemosensitive and 17 chemorefractory. Nine were in CR at the time of allo-HSCT. Twenty-five had matched related donors, 3 mismatched related, 2 matched unrelated, and 1 mismatched unrelated donors. Stem-cell source was bone marrow in 11 and mobilized peripheral blood in 21. Conditioning regimens were myeloablative (n=26) and non-myeloablative (n=6). Total body irradiation was given to 23 patients.
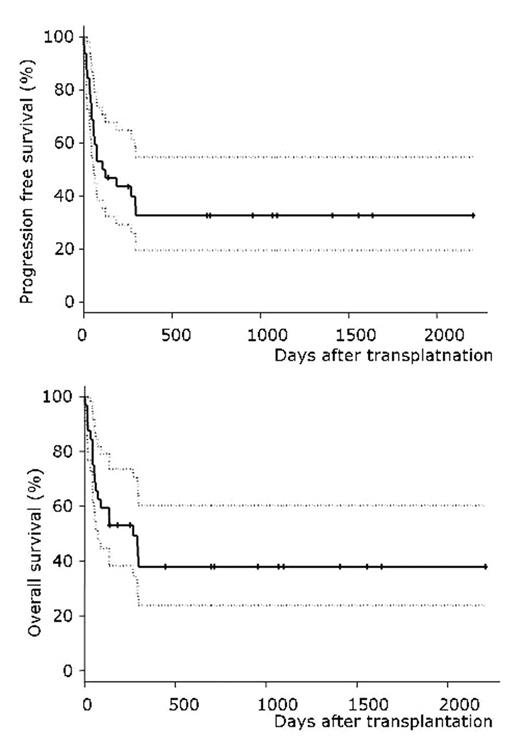
Graft-versus-host disease (GVHD) prophylaxis was cyclosporin and short-term methotrexate in 27 patients. Grade 2–4 acute GVHD and chronic GVHD developed in 13 and 9, respectively. Nine died of disease progression, 4 of infection, 2 of veno-occlusive disease, 2 of acute GVHD, 1 of interstitial pneumonitis, and 1 of thrombotic microangiopathy. Two-year progression-free and overall survivals were 33% and 38%, respectively (median follow-up, 32 months). All patients who did not relapse/progress within 10 months achieved progression-free survival during the follow-up. In multivariate analysis, stem cell source (BM vs. PB; relative risk 3.33) and acute GVHD (grade 2–4 vs. grade 0–1; relative risk 2.56) significantly affected progression-free survival. Allo-HSCT is a promising treatment for NK-cell neoplasms.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal