Abstract
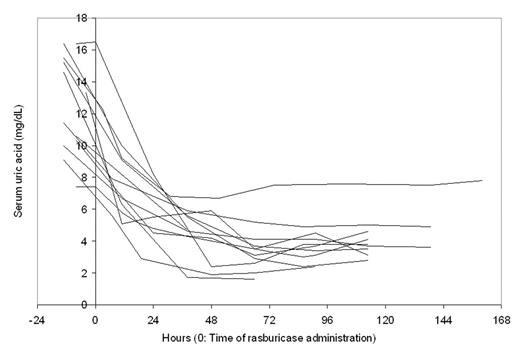
Hyperuricemia is a feature of tumor lysis syndrome (TLS), and is treated with hydration, urine alkalinization, and allopurinol. Allopurinol inhibits the conversion of hypoxanthine to xanthine, and xanthine to uric acid (UA) by inhibiting xanthine oxidase. It has no direct effect on existing UA. Rasburicase lowers UA rapidly to very low levels at the labeled dose of 0.15–0.2 mg/kg daily for 5 days by converting UA to allantoin which is rapidly excreted. Despite this dramatic effect on UA, rasburicase has not been shown to have any beneficial impact on survival. We administered 0.2 mg/kg ideal body weight rasburicase to an obese hyperuricemic patient (actual 120 kg, ideal 60 kg). Serum UA declined from 11 mg/dL to 1.4 mg/dL in 3 h and 0.4 mg/dL in 11 h. The serum UA level remained low for several days and a second dose was not needed. After seeing this dramatic and sustained response, low rasburicase doses were used in patients with malignant diseases with close monitoring of biochemical parameters. No dose level was systematically explored and the doses used ranged from 1.5 mg to 12 mg. This analysis is a retrospective review of all patients who received low-dose rasburicase. 23 adults (39–78 y) with cancer and hyperuricemia received a single low dose of rasburicase at 12 mg (n=1; index case), 6 mg (n=2), 4.5 mg (n=1), 3 mg (n=18), and 1.5 mg (n=1). 6 patients received 1 and 1 patient received 2 more doses of 3 mg each. Allopurinol and other supportive therapy including hydration were administered. UA levels (baseline 7.4–19 mg/dL, median 11.6) declined by 4–96% (median 40%) within 24 h of rasburicase administration (Fig 1; the dashed lines show patients receiving more than 1 rasburicase dose).
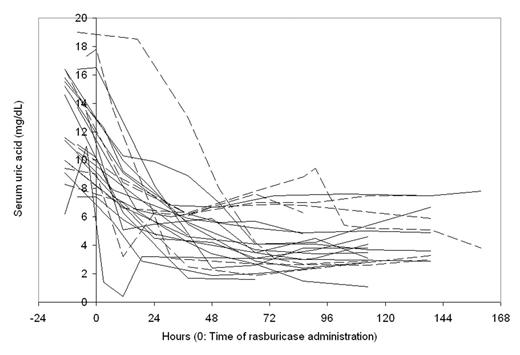
The decline was 31–68% (median 46%) amongst the 12 patients receiving a single 3 mg dose (Fig 2).
The baseline serum creatinine was 0.9–8.4 mg/dL (median 2.4), and the minimum and maximum values in the week following rasburicase were 0.7–5.8 (median 1.8) and 1.0–8.8 (median 2.6) respectively. No clinically significant renal dysfunction developed in any patient. The total rasburicase dose administered, 3–12 mg (median 3 mg), was 3–12% (median 5%) of the recommended dose. Based on the Red Book rasburicase cost of $387 for a 1.5 mg vial, the amount of money saved ranged from $11,000 to $29,000 per patient; for a total saving of between $373,000 and $507,000. While this was not a systematic dose-reduction study and patients were treated by multiple physicians and pharmacists on clinical grounds, the data suggest that rasburicase is effective at a fraction of the recommended dose. While a formal investigation of low doses is warranted, we recommend using rasburicase at a standard dose of 3 mg in hyperuricemic patients, checking UA levels frequently, and repeating rasburicase administration if needed. This approach has the potential for substantial cost saving while providing appropriate therapy to lower UA.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal