Abstract
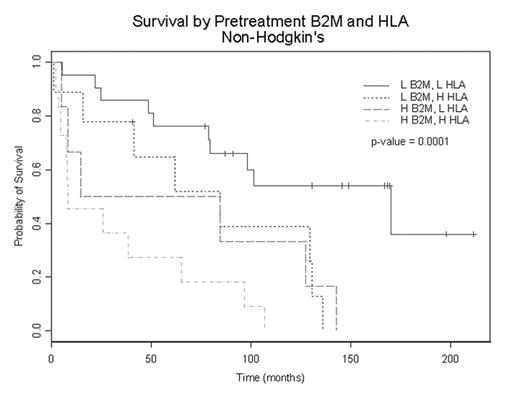
Higher levels of b-2 microglobulin (b2-M) have been reported to correlate with poor outcome in non-Hodgkin’s lymphoma (NHL) and Hodgkin’s disease (HD). However, b2-M is a subunit of the human leukocyte antigen-class I (HLA-I) molecule, which is composed of b2-M and the alpha heavy chain. Although soluble HLA-I (sHLA-I) protein has been detected in circulation and is believed to play a role in immunomodulation by inducing apoptosis in cytotoxic T-lymphocytes, the clinical relevance of sHLA-I levels in HD and NHL is not known. Here we report that serum sHLA-I levels are increased in NHL and HD. More importantly, levels of sHLA-I correlate with clinical behavior in NHL in a fashion similar to that of b2-M. In a multivariate model incorporating b2-M, sHLA-I, and IPI (International Prognostic Index), NHL patients with sHLA-I levels >312.60 mg/mL had significantly shorter survival than those with lower levels, independent of IPI score. Moreover, a model incorporating both sHLA-I (cut-point = 312.60 mg/mL) and b2-M (cut-point = 4.16 mg/L) levels were highly predictive of survival (Figure) in NHL patients. In contrast, in HD, b2-M levels correlated with clinical behavior whereas HLA-1 levels did not. These data not only establish the role of sHLA-I as an independent tumor marker in NHL that can be used to stratify patients, but also suggest that, in HD, b2-M and sHLA-I may reflect different processes. The role of sHLA-I as an immunomodulator may be responsible for its divergence from b2-M as an indicator of clinical behavior in HD. Further studies exploring the importance of this role in the biology of HD are needed.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal