Abstract
<Introduction>The potential role of RICBT in adults remains unclear. This study reports the results of RICBT for adults with hematological diseases.
<Objective>The 1st purpose of this report was to investigate the risk factors of non-relapse mortality (NRM) within day 100 of RICBT and the 2nd was to identify its prognostic factors.
<Patients and Methods>We reviewed medical records of 107 patients with advanced hematological diseases who had received RICBT between March 2002 and June 2004 at Toranomon Hospital, Tokyo, Japan. Median age of the patients was 55 years (17–79). Primary diseases were advanced (n=88) or standard (n=19). Median follow-up was 14 months (0.5–27). Conditioning regimen was fludarabine 125 mg/m2, melphalan 80 mg/m2 and TBI 4 Gy. GVHD prophylaxis was cyclosporine (n=87) or tacrolimus (n=26). Median total nucleated cells (TNC): 3.2 x 10^7 cells (1.7–4.3); Median CD34+: 1.4 x 10^5 cells (0.21–3.28); HLA match: 6/6 (n=4), 5/6 (n=3), 4/6 (n=95), 3/6 (n−1). Time to event curves were plotted by using the actuarial method of Kaplan-Meier, and differences between curves were analyzed by log-rank tests. The following factors were considered potential predictors of outcomes about 1st and 2nd purpose: age, weight, sex, risk, HLA disparities, TNC, CD34+, GVHD, pre-engraftment reactions (PER) that we have reported (Clin Cancer Res.10:3586-92, 2004), and use of steroids for PER. All factors were tested for the proportional hazards assumption.
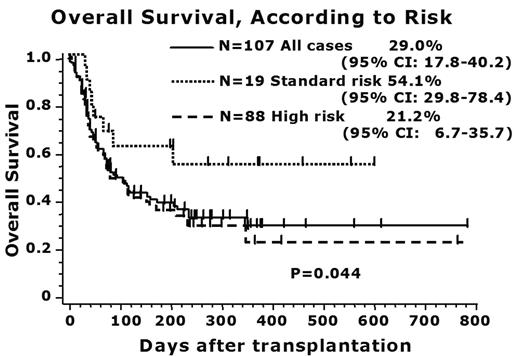
<Results>Neutrophile (>500/μL) and platelet recovery (>20,000/μL) were observed in 77.9% at day 60 (median; 19.5 day), 48.7% at day 100 (45.5 day), respectively. Primary graft failure was occurred in 8% of all cases. Cumulative incidence of acute GVHD (II-IV) and chronic GVHD were 39.8% and 21.1%, respectively. Causes of NRM included infections (n=30), regimen related mortality (RRM) (n=19), and GVHD (n=6). Incidence of NRM at day 100 was 51.6% (95% CI: 42–61), 33 patients with use of steroids for PER had NRM at day 100 of 75% (95% CI: 67–94), as compared to 39% (95% CI: 25–48) in 77 patients without use of steroids (p<0.05). The estimated OS was 29.9% (95% CI: 17.8–40.2) in all cases, 54.5% (95% CI: 29.8–78.4) in standard, and 21.2% (95% CI: 6.7–35.7) in advanced (p<0.05), respectively. In multivariate analysis, the most important risk factor of NRM was use of steroids for PER (p<0.05), while other factors did not influence. As for OS, disease status and use of steroids for PER were significant predictors of OS (p<0.05).
<Discussion and Conclusion> RICBT is associated with a high NRM. This study has demonstrated status of underlying diseases and use of corticosteroid for PER as a significant prognostic factor. Eligibility of RICBT needs to be investigated, and further studies are warranted to clarify the pathogenesis of PIR and its optimal management.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal