Abstract
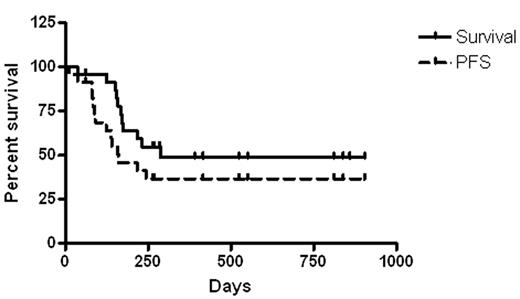
Non-myeloablative conditioning has extended the use of allogeneic hematopoietic transplant to many previously ineligible patients but has to date been disappointing in patients with advanced acute myelogenous leukemia (AML). We added the immunosuppressive and antitumor agent sirolimus (rapamycin) to an established transplant regimen of fludarabine 25 mg/M2 days -7 through -3 and cyclophosphamide 1000mg/M2 days −7 and −6, with tacrolimus and methotrexate immunoprophyllaxis. 23 patients with AML were treated, with median age 59 (range 28–72) at transplant. 6 patients received matched sibling, 11–unrelated donor, 1–5/6 matched and 5-haploidentical (“haplo” −3/6 or 4/6 matched) transplants. The haplo recipients also received antithymocyte globulin on days −1, 1, 3, and 5. Only 7 patients in total were in CR, but all of these were at high risk for relapse because of prior MDS, chromosome status, or other features. 9 patients were in chemotherapy refractory progression, and 7 were primarily refractory to induction therapy. All patients engrafted. In patients without graft versus host disease by day 30 (9 patients) tacrolimus was discontinued between days 45 and 100 while sirolimus was continued. 12/23 patients survive at 61–903 days of followup post transplant (median 525) and 11/12 survivors are currently free of detectable leukemia. 3 of these 12 relapsed at 83, 88, and 243 days, but the first 2 of these have received chemotherapy and DLI and are in CR 771 and 311 days from relapse. The figure below shows overall and progression free survival (PFS). All survivors but the single patient undergoing therapy for progression have performance status 0 or 1 and are free of need for transfusion. 9/12 survivors continue on sirolimus therapy. Only 2 patients, both recipients of haploidentical cells, have died from transplant related causes. Non-myeloablative hematopoietic cell transplantation with sirolimus (rapamycin) based immunosuppression effectively treats many patients with advanced and poor prognosis AML. Given the very limited anti-leukemic activity of the conditioning chemotherapy, this suggests that disease control has been via graft versus leukemic effects alone or combined with anti-leukemic activity of the sirolimus.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal