Abstract
56 adults with hematologic malignancies underwent blood cell allografts from A/B-DR-identical MSDs or A/B/C/DRB1/DQB1-allele-identical MUDs after 100 mg/m2 melphalan with (n=39; no prior autograft) or without (n=17; prior autograft) 50 mg/kg cyclophosphamide. GVHD prophylaxis comprised mycophenolate with cyclosporine (MSD) or tacrolimus (MUD). No growth factors were used. Supportive care was uniform. There were significant differences between groups (Table 1); most strikingly with respect to donor age.
| . | MSD (n=37) . | MUD (n=19) . | P . |
|---|---|---|---|
| Pt age | 53 (38–66) | 47 (27–62) | 0.085 |
| Pt age >55 | 32% | 32% | 0.95 |
| Donor age | 51 (31–69) | 33 (24–50) | <0.0001 |
| Donor age >45 | 76% | 16% | <0.0001 |
| Refractory disease | 49% | 68% | 0.16 |
| PS 2–3 | 22% | 32% | 0.42 |
| LDH | 172 (83–1298) | 237 (105–1919) | 0.082 |
| Abnormal LDH | 43% | 63% | 0.16 |
| CD34+ cell dose | 5.0 (3.0–7.6) | 6.0 (1.4–11.8) | 0.12 |
| CD34+ cell dose >6 | 11% | 47% | 0.002 |
| . | MSD (n=37) . | MUD (n=19) . | P . |
|---|---|---|---|
| Pt age | 53 (38–66) | 47 (27–62) | 0.085 |
| Pt age >55 | 32% | 32% | 0.95 |
| Donor age | 51 (31–69) | 33 (24–50) | <0.0001 |
| Donor age >45 | 76% | 16% | <0.0001 |
| Refractory disease | 49% | 68% | 0.16 |
| PS 2–3 | 22% | 32% | 0.42 |
| LDH | 172 (83–1298) | 237 (105–1919) | 0.082 |
| Abnormal LDH | 43% | 63% | 0.16 |
| CD34+ cell dose | 5.0 (3.0–7.6) | 6.0 (1.4–11.8) | 0.12 |
| CD34+ cell dose >6 | 11% | 47% | 0.002 |
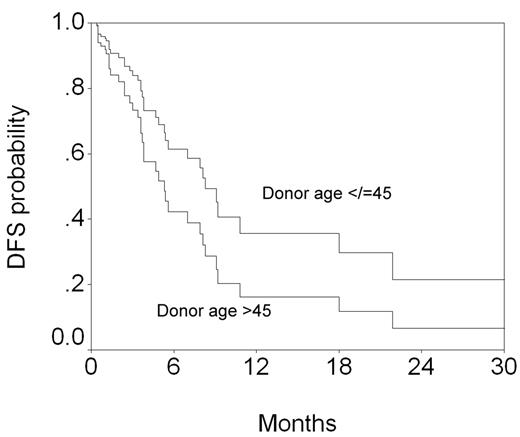
10 patients experienced transplant-related mortality (TRM), and 29 relapsed (23 dead). The following factors were analyzed in a Cox model for effect on outcome: chemosensitive (n=25) vs refractory disease (n=31), patient age ≤55 (n=38) vs >55 (n=18), performance status (PS) 0–1 (n=42) vs 2–3 (n=14), normal (n=28) vs abnormal (n=28) LDH, prior autograft or not, CD34+ cell dose ≤6 (n=43) vs 6 (n=13) x 106/kg, MSD vs MUD, male (n=38) vs female (n=18) donor, and donor age ≤45 (n=25) vs >45 (n=31). Donor age was also analyzed as a continuous variable. Patient age >55 and PS 2–3 resulted in higher TRM. Refractory disease and abnormal LDH resulted in higher relapse, and lower disease-free (DFS) and overall (OS) survival. PS 2–3 resulted in lower DFS and OS. Patient age >55 and MSD resulted in lower OS. OS was reanalyzed after excluding donor type as a variable (*) because of its correlation with donor age. Table 2 shows the favorable effect of donor age ≤45 on relapse, DFS and OS.
| Outcome . | RR (95% CI) . | P . |
|---|---|---|
| Relapse | 0.28 (0.12–0.64) | 0.003 |
| DFS | 0.27 (0.13–0.57) | 0.001 |
| OS* | 0.42 (0.19–0.94) | 0.035 |
| Outcome . | RR (95% CI) . | P . |
|---|---|---|
| Relapse | 0.28 (0.12–0.64) | 0.003 |
| DFS | 0.27 (0.13–0.57) | 0.001 |
| OS* | 0.42 (0.19–0.94) | 0.035 |
When analyzed as a continuous variable, lower age resulted in lower relapse and higher OS with donor type in the model, and with higher DFS when donor type was excluded. Figures 1 and 2 show the effect of donor age on relapse and DFS in plots generated from the Cox model at the means of the covariates.
These data appear to suggest that a young MUD may be preferable to an older MSD. However, small numbers preclude obtaining an answer to the question of the age at which a sibling donor should be considered too old. Additionally, logistic issues involved in obtaining a MUD may reduce any benefit from having a young donor. We conclude that a younger donor should be chosen whenever possible. Further work is required to address the intrguing possibility of superiority of MUD over MSD based on age.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal