Abstract
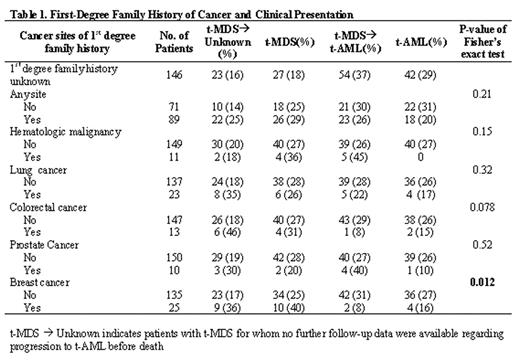
Therapy-related myelodysplastic syndrome (t-MDS) and therapy-related acute myeloid leukemia (t-AML) occur in a subset of patients treated with chemotherapy and/or radiation for various primary malignancies. Whether or not a patient develops t-MDS/t-AML can be influenced by a combination of genetic and environmental factors. We conducted a retrospective analysis of t-MDS/t-AML patients who had cytogenetic analyses performed at the University of Chicago Hospitals between 1972 and 2001 to determine if a family history of cancer could be associated with t-MDS/t-AML development. These included 141 males and 165 females whose median age was 51 years (range was from 3–83 years) at the time of primary diagnosis and 58 years (range was from 6–86 years) at the time of t-MDS/t-AML presentation. Out of 306 patients, data on first-degree family history of cancer was documented in 160 patients, but there was no statistically significant difference in the characteristics examined below between patients with self-reported family history of cancer and patients with undocumented family histories. A first-degree family history of any cancer was reported in 89 patients (55.6%). The prevalence of family history of specific sites were: 25 (15.6%) of breast cancer, 23 (14.4%) of lung cancer, 13 (8.1%) of colorectal cancer, 11 (6.9%) of hematologic malignancy, 10 (2.3%) of prostate cancer, 6 (3.8%) of stomach cancer, 5 (3.1%) of uterine cancer, 5 (3.1%) of CNS cancer, 5 (3.1%) of pancreas cancer, 4 (2.5%) of melanoma, 3 (1.9%) of oral-pharyngeal cancer, 3 (1.9%) of ovarian cancer, 3 (1.9%) of cervical cancer, 2 (1.3%) of vulvar cancer, 1 (0.6%) each of bladder cancer, sarcoma, renal cancer, or esophageal cancer. Of note, only a family history of breast cancer was associated with clinical presentation as show in Table 1 below. Patients with a family history of breast cancer were also more likely to have a chromosome 5 and/or 7 abnormality (84%) than patients without (62%, p=0.04). There was no significant association between family history of cancer at other sites and clonal cytogenetic abnormalities. A subgroup analysis was conducted in patients with a primary diagnosis of breast or ovarian cancer. Of the 24 patients who had data on family history of cancer, 16.7% reported having a first degree relative with breast cancer. These findings suggest a possible genetic component linking family history of breast cancer and development of t-MDS/t-AML, as was previously reported by Rauscher et al. (2002) for de novo adult leukemia incidence. Further studies of family histories of cancer, in particular breast cancer among patients receiving chemotherapy and/or radiation, could potentially elucidate the genetic basis of leukemia and ultimately lead to new tools for risk assessment, early detection or prevention of secondary leukemia in cancer survivors.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal